Removing the Materials Handcuff on Medtech
Explore the potential of new materials for medical devices at MD&M West’s 2022 Design. Engineer. Build conference in the April 12 session, Designing with Biomaterials for Better Medical Outcomes.
April 4, 2022
James Biggins, CEO of Access Vascular Inc.
Today, innovation efforts by medical device and medtech companies are significantly handcuffed by a scarcity of new base materials available for novel product design and production. To realize breakthrough clinical and economic improvements on today’s standards of care, we must find a way to remove these logjams.
Why Materials Choice Matters for Medical Devices
Empty grocery store shelves during the pandemic provide an interesting parallel to the material constraints faced by medical device companies. Having only whole grain sliced bread available for purchase at the supermarket can lead to a wide variety of cascading consequences for consumers. Those on a budget might have to buy fewer groceries than planned. Others might have to abstain altogether.
Similarly, a limited selection of materials available for use in medical devices forces hard decisions on engineering teams. For instance, would the team need to use a polymer with suboptimal performance that necessitates a larger-sized, more invasive device? Or would it select a material that might not be resistant to the intended biological environment for the duration of the therapy?
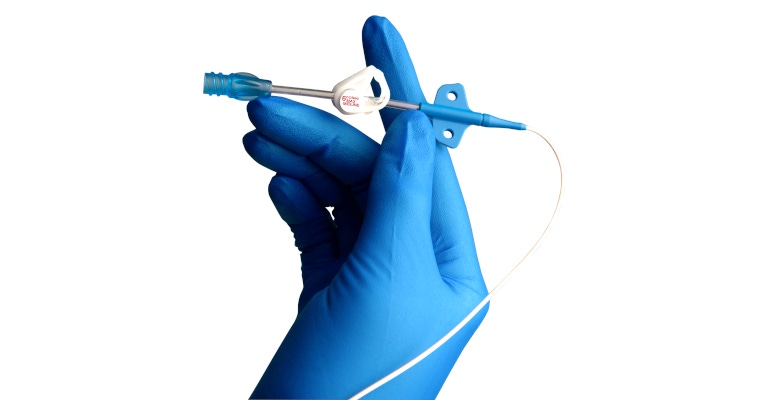
Unfortunately, these tough choices are routine for medtech companies and play out every day in hospitals around the country. Consider vascular access catheters.
Polyurethane has formed the core of nearly every catheter produced in the United States since the 1970s. We know that this material can trigger the body’s natural defenses, leading to a cascade of complications such as thrombosis, infection, even death. This happens in an astounding 30% of cases where a catheter is inserted (most hospital inpatients receive some type of catheter).
We also know that the base material makes a difference because the use of biomaterials in catheters has been shown to nearly eliminate these complications. Yet, most catheters continue to rely on polyurethane because it is the easy, approved material of choice.
The tide will likely turn in the case of catheters, but there is a litany of other medical devices and applications that are still handcuffed by a lack of new materials. I’m reminded of the birth control device Essure, which was the subject of the controversial Netflix special “The Bleeding Edge.”
Bayer stopped selling Essure in the United States at the end of 2018, citing a decline in U.S. sales of the device and the conclusion that the Essure business was no longer sustainable, MD+DI reported. However, a study suggests the materials used in the design could have led to some adverse patient events. Could the availability of new, more beneficial materials have avoided this outcome and allowed the device to remain on the market as a compelling option for women? Perhaps.
Roadblocks to Materials Innovation
Today, makers of medical devices are largely limited to thermoplastics and high-grade metals. There are exceptions, such as the novel hydrophilic biomaterial we use in our own catheters, but most engineers must choose between one of these widely available types of materials.
This limited selection results from two primary reasons: perceived liability from material manufacturers and a gap between how the industry and regulators view new materials. These concerns lead to even compelling, decades-old materials being sidelined because they are still undergoing required research and testing protocols.
Liability is a valid concern for developers and suppliers of new materials. The $4.25 billion Dow Corning settlement because of faulty silicone breast implants certainly serves as a warning. Given the enormous size of the medical market, suppliers are extremely cautious and work aggressively to limit their exposure. For example, engineers sourcing new materials must disclose the intended end-use for the materials. If they list “medical device” on the application, they are often denied even samples for prototyping or other research efforts.
The disconnect in regulatory approval is often because of a lack of clarity on the part of industry. FDA continues to make significant adjustments to how it regulates materials used in new products, making it easier for companies to implement new materials.
This is in part because of updates from the International Organization of Standardization (ISO)—which is leveraged by FDA—regarding the chemical characterization of materials used in medical devices. New ISO updates help inform a remarkably sensible modernization of the regulations that align testing, maintenance, and safety standards with the industry’s need for cost and efficiency.
However, industry still lags in its understanding and utilization of these changes. Most follow a path of least resistance and slot in previously approved materials as part of device applications to avoid perceived approval barriers.
It's now on medtech designers and companies to better understand these changes and adapt their regulatory strategies and testing practices accordingly. A great first step would be to educate engineers and designers on the updates and how to leverage them in their own work.
These initial adaptations will gradually lead to industry-wide adjustments and eventual best practices for entering new materials into design standards. The result will be expedited approvals and next-generation products benefiting patients.
Remaking Medicine Through Materials
Ultimately, broader materials selection is critical to the future of medtech.
No one is advocating that we put untested materials into medical use, but there is a common-sense approach to testing and evaluating materials that will allow us to break this logjam and realize gains clinically and economically at a time when both are sorely needed.
By understanding and adapting to new regulatory changes, the industry can speed approvals for new materials and ensure safety at the same time. The key is not to default to prior standards and materials through ignorance.
Embracing new materials will enable medtech to build on recent biomaterial innovations like resorbable technology and hydrogels. Instead of serving as the bleeding edge of innovation, these advances will simply become the foundation for an entirely new generation of materials with the potential to transform patient care and outcomes.
Register for MD&M West here to attend Jim’s April 12 session at the Design. Engineer. Build. Conference, "Designing with Biomaterials for Better Medical Outcomes." The event serves as the meeting point for engineers, disruptive companies, and innovative thinkers to create powerful solutions and life-changing medical devices.
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
