New Tools for Preventing Hospital-Acquired Infections
As the focus on hospital-acquired infections intensifies, some medical device manufacturers are considering deep UV light emitting diodes for smaller, portable disinfection devices. Here's how the technology can be used in medical device design.
October 19, 2016

As the focus on hospital-acquired infections intensifies, some medical device manufacturers are considering deep UV light emitting diodes for smaller, portable disinfection devices. Here's how the technology can be used in medical device design.
Mark Pizzuto

According to the Centers for Disease Control and Prevention (CDC) one in every 25 hospital patients in the United States will contract a hospital-acquired infection (HAI) during their visit. Often expensive and sometimes fatal, HAIs are adding billions to the country's already skyrocketing healthcare costs.
For decades, hospitals and other healthcare facilities have relied on ultraviolet germicidal irradiation (more recently referred to as germicidal UV, or GUV) systems equipped with low pressure mercury vapor lamps to disinfect everything from operating rooms to the air circulating in the building's ductwork.
Learn more about "What You Need to Understand about Health Systems to Design Your Business and Product Strategy" at BIOMEDevice San Jose, December 7-8. |
For the most part, these systems provide an increased level of disinfection. However, low-pressure mercury lamps emit light at a spectral peak wavelength of 253.7 nm. Though effective, the wavelength is not optimal from a germicidal efficiency standpoint. More importantly, due to their size and fragility, the lamps cannot address the healthcare industry's growing need for smaller, portable UV disinfection devices.
As an alternative, medical device manufacturers are turning to deep UV (UVC) light emitting diodes (LEDs), which offer a much smaller footprint as well as UVC light in the optimal 250-280 nm wavelength range. While the small footprint provides designers with unparalleled flexibility, they can also adjust the LED's input drive current to optimize the light intensity and create customized disinfection tools that directly support and improve a healthcare facility's HAI prevention protocols.
Developing New, Portable Solutions
Consistent with the growing shift from managed care to a more decentralized model, leading medical device manufacturers are developing innovative new solutions to safeguard both patients and clinicians from harmful drug-resistant pathogens and life threatening infections. At the end of 2015, the newly signed federal budget temporarily suspended the 2.3% excise tax on medical devices for the next 24 months, in part allowing device manufacturers, both public and private, to resume R&D programs.
Ultraviolet (UV) disinfection is a reliable and viable alternative to chemical disinfection methods because it disrupts the DNA of harmful microorganisms and destroys their ability to reproduce--thereby eliminating the spread of MRSA, C. difficile (C. diff), staph, and many other pathogens. The C. diff spore, which can remain active on surfaces for up to three months and is the most difficult to kill, is generally regarded as the benchmark for confirming new disinfection process efficacy.
From a system or portable instrument perspective, UVC LEDs are a major upgrade. They can deliver UVC light in optimal wavelengths for targeted disinfection and they have a much smaller footprint, consuming far less energy due to their instant on/off operation. As a result, designers are able to develop new and increasingly portable GUV disinfection instruments that can do a better job preventing the spread of infection at the hospital, community care facilities, or in the home.
Variation in Required UV Dosage by Microbe
UV disinfection relies on radiation emitted in the wavelength range of 250 nm to 280 nm to inactivate pathogens by breaking their DNA strand. Following a number of important advancements in semiconductor-based UVC LED technology, LEDs are now viewed as a viable, cost-effective, and environmentally friendly alternative to mercury-based lamp technologies.
As interest in UVC LEDs continues to grow, medical device/system designers looking to develop new products must first focus on the log reduction target to optimize the UV dosage for their application. Log reduction is a mathematical term used to show the relative number of live microbes that are eliminated from a surface by disinfecting or cleaning.
For example, a "4-log reduction" lowers the number of microorganisms by 10,000-fold--if a surface contains 10,000 pathogenic microbes, a 4-log reduction would reduce the number of microorganisms to one.
By establishing the log reduction target for an application first, designers can then determine the distance from the light source and time of exposure that's needed to achieve it. Or, to put it another way, the distance from the UVC energy, combined with the amount of time the surface is exposed to the UVC light, will directly determine the level or degree of disinfection.
Experiments recently conducted at EMSL, a third-party microbiological testing facility in New York, targeted common microbes for UVC LED disinfection applications (Table 1). The goal was to measure the level of disinfection achieved on different microbes across a range in gram positive, gram negative, and fungi groups as a function of time and distance.
Microbe | Type |
MRSA | Gram + Bacteria |
Staphylococcus aureus | Gram + Bacteria |
Staphylococcus epidermidis | Gram + Bacteria |
Enterococcus faecelis | Gram + Bacteria |
Pseudomonas aeruginosa | Gram - Bacteria |
Acinebacter baumanii | Gram - Bacteria |
Clostridium difficile | Gram + Bacteria (spore forming) |
Candida albicans | Fungi |
The log reduction for each microbe was measured after being exposed to UV at intervals of 30, 60, and 120 seconds. The exposure data can be seen in Figures 1 and 2 at distances from the light source of 2 inches and 3.5 inches respectively. After 120 seconds of exposure at a distance of 2 inches, there was slightly more than a 5.3 log reduction on all the gram positive bacteria with a 6 log reduction for MRSA. Bacteria of gram negative types experience a log reduction value between 4 and 5; fungi had a log reduction value of approximately 3 and gram positive (spore forming) experienced just over a 1 log reduction.
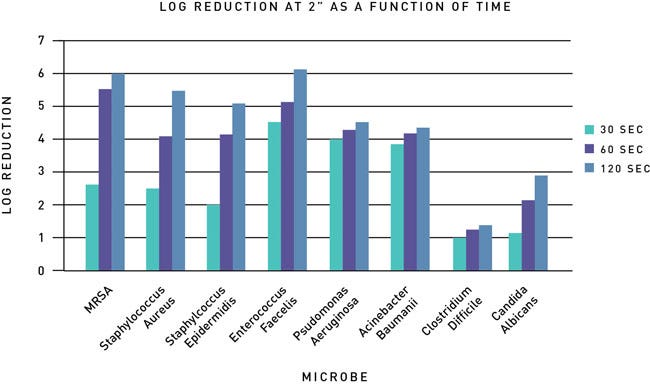
Fig 1: Log reduction as a function of time for various microbes at 2" distance.
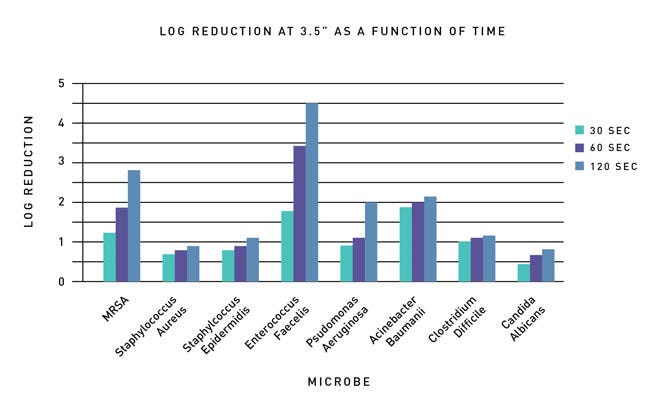
Fig 2: Log reduction as a function of time for various microbes at 3.5" distance
At a distance of 3.5 inches, the log reduction follows a similar trend, albeit less powerful, for the gram negative and fungi microbes. The gram positive and gram positive (spore forming) microbes follow a less predictable pattern with the increase in distance. This may be attributed to the dosage required for complete inactivation of the microbe.
These experiments clearly demonstrate that when the distance is increased and time and UVC power are held constant, the log reduction is lower. However, this decrease in disinfection occurs in an unpredictable fashion, indicating that while dosage calculations provide guidance on application design, true verification of log reduction values must be validated through microbiology studies.
Achieving Uniform Disinfection with Design Flexibility
Complete exposure of a surface will allow for delivery of optimal dosage. The compact footprint of UVC LEDs enables better disinfection of small or irregular-shaped surfaces. By leveraging the much smaller LED footprint, new disinfection devices can be created to match the shape of the intended target.
Figures 3 and 4 illustrate how LEDs can be used to disinfect two surfaces--a cylindrical vial and a small workstation. As UV disinfection is line-of-sight irradiation, the LEDs can be configured to deliver uniform light dispersion across two very different surfaces.
In Figure 3, a cylindrical vial requires a dosage of 5 mJ/cm2, which must be achieved at the furthest point from the LED array--the base of the vial 81 mm from the light source. While the irradiation will be higher on the sidewalls near the top of the vial, delivering the minimum dosage to the base ensures the entire vial surface is disinfected. Based on the modeling data, this arrangement achieves the required dosage after 10 seconds.
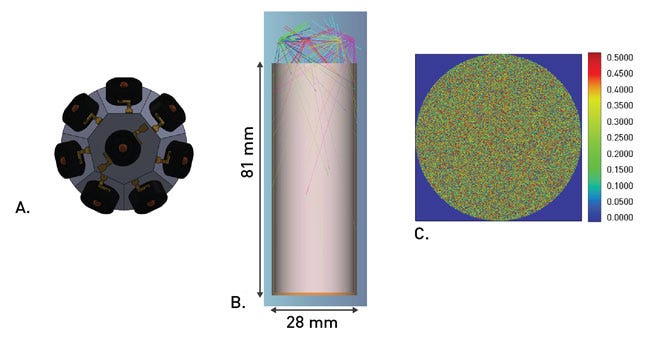
Figure 3: Arrangement of LEDs that can be used for disinfection of vials (A), the optical modeling of the irradiation of the vial (B), and the irradiation pattern at the bottom of the vial (C).
Figure 4 illustrates the disinfection of a workspace surface 100 mm wide (about 4 inches), requiring a dosage of 12 mJ/cm2. The LEDs are arranged in a 100 mm wide strip of four UVC LEDs set approximately 25 mm above the surface. To achieve a uniform dispersion with the 100-degree viewing angle of the LEDs, they must be placed 25 mm apart in the array. The target dosage can be achieved by irradiating the surface for 60 seconds.
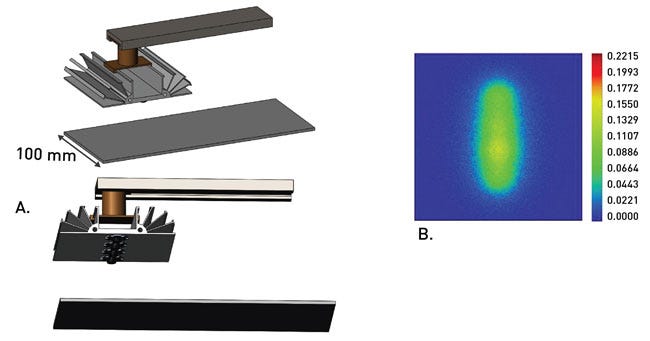
Figure 4: Arrangement for surface disinfecting bar that can move along the axis (A) and radiation pattern from the LED on to a surface in stationary mode (B).
Being able to arrange LEDs to accommodate a specific surface enables medical device engineers to create a whole new generation of reliable devices that deliver uniform and highly efficient UV disinfection. As a result, instrument manufacturers can develop new and, when necessary, customized instruments for specific high-contact surfaces.
Beyond the Design Benefits of UVC LEDs
According to the CDC, microorganisms and viruses have developed numerous resistance mechanisms that enable them to evade the effect of antimicrobials and antivirals, suggesting many have become resistant to almost every available means of chemical treatment--all of which contributes to the rise in HAIs. The need to protect hospital patients and clinicians from harmful, drug resistant pathogens and life-threatening infections has, therefore, never been greater.
For hospitals and other healthcare providers, a high incidence of HAIs can also result in significant financial penalties. Under the Affordable Care Act's Hospital-Acquired Condition Reduction Program, healthcare providers that fail to achieve successful patient outcome targets can suffer reduced reimbursements for their services.
Global spending on infection control--which includes chemical and physical disinfection equipment--is projected to grow from $13.1 billion in 2014 to $16.7 billion by 2020. Not surprisingly, the fastest growing segment includes new systems and devices that employ UVC LEDs for repeatable, reliable, and environmentally safe disinfection.
Looking ahead, healthcare providers, medical device OEMs, and disinfection equipment manufacturers alike have every reason to embrace smaller, portable devices that employ solid-state technology like UVC LEDs. Doing so will significantly bolster what's projected to be a long and difficult fight against the spread of infectious diseases and the ongoing emergence of chemical-resistant super bugs.
Mark Pizzuto is director of product management, disinfection at Crystal IS. Based in Green Island, NY, Crystal IS is a manufacturer of UVC LEDs.
[Image courtesy of RENJITH KRISHNAN/FREEDIGITALPHOTOS.NET. Figures courtesy of CRYSTAL IS.]
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
