AirStrip’s Push to Mobilize Medical Data
AirStrip Technologies (San Antonio) is a pioneer in the field of mobile patient monitoring.
November 9, 2012
AirStrip Technologies (San Antonio) is a pioneer in the field of mobile patient monitoring. The company’s first product, AirStrip OB debuted in 2006, giving obstetricians access to live remote monitoring of expectant mothers on their mobile devices. It was the first FDA-cleared medical application to be included in Apple’s App Store.
|
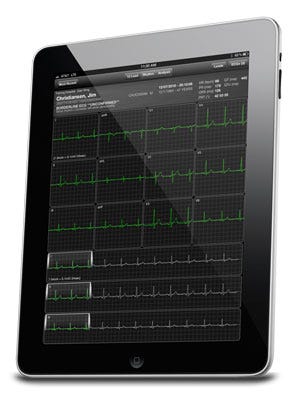
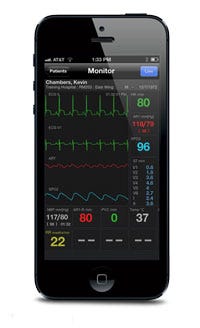
The AirStrip platform was the first FDA-cleared product to be included in Apple's App Store. |
Following that, the company rolled out patient monitoring and cardiology platforms. At present, the company’s technology is now in use in more than 400 hospitals across the world.
Citing the technology’s capabilities in maternal fetal monitoring, cardiology, and patient monitoring, Leslie Saxon, MD, a professor of clinical medicine at the USC Keck School of Medicine, says that “AirStrip has developed software products that are really meaningful that solve major problems.”
Building on that point, Daniel Kraft, MD, chair of the medicine track at Singularity University and executive director of FutureMed, says, “As medicine and healthcare become increasingly digital, mobile, and connected, platforms like the one AirStrip has pioneered can generate critical actionable information, leading to better outcomes at lower costs and higher convenience.” Kraft points out that the platform enables physicians to obtain relevant information in real time and access dashboards that can filter and intelligently present data to the clinician.
The ability to beam patient data wirelessly to physicians isn't only convenient; it also helps address a key problem: the shortage of caregivers. The United States alone is projected to have nearly 63,000 fewer doctors than it needs by 2015, based on estimates from the Association of American Medical Colleges.
The Dawn of the Virtual Physician
|
Alan Portela, AirStrip Technologies' CEO |
A study released late in 2011 by CompTIA found that more than half of physicians use a smartphone for work purposes and that number is expected to steadily rise. In 2012, physician mobile use increased by 45%, according to a Bulletin Healthcare study. “Physicians are becoming mobile professionals, and you need to create the concept of a virtual physician,” says Alan Portela, CEO of AirStrip Technologies.
“You need to look at their entire workflow and figure out how to mobilize all of the components that physicians need in order to support their workflow.”
Recently, the firm has shifted its focus from solely developing healthcare apps to an enterprise-wide solution suite. “We figured out that if we want to really support the workflow of physicians and bring disruptive innovation to the industry, we need to mobilize the two most important clinical data sources: medical devices and EMR/EHRs," Portela says.
To add electronic medical record (EMR)-mobilizing capabilities to its suite of HIPAA-compliant products, the company acquired a mobile EMR extender developed by Palomar Healthcare (Escondido, CA). “They developed the same thing that we did for mobile medical devices for EMR,” Portela says. “They created an agnostic native mobile EMR extender that has the ability to connect to Cerner, Meditech, McKesson, and other EMR systems and provide a single consolidated view of the EMR data." Airstrip acquired intellectual property for the technology and plans to integrate both the mobile EMR extender and mobile medical device access capability before the end of 2012.
Portola is also looking for third-party vendors to capture images. "We want to be able to mobilize DICOM images so you have medical devices, EMRs, and medical images as part of a single, fully integrated solution.” The EMR systems will use military-grade encryption technology.
Cutting Costs and Improving Quality of Care
The technology can help improve quality in critical care, cardiology, and obstetrics by quickly alerting remote clinicians when there is a problem. Consider, for instance, how the technology can help a patient who has suffered a heart attack.
|
AirStrip's platform enables clinical data to be viewed on the iPad, iPhone, and a variety of other mobile platforms. |
“Say we are dealing with a ST-segment-elevation myocardial infarction (STEMI)—a complete blockage of the artery,” Portela says. “What happens today is that many of those patients basically get picked up by the ambulance and the event to balloon time is somewhere between 90 and 120 minutes. That is the national standard door-to-balloon time, from the emergency department to the cath lab.”
By contrast, the following scenario is made possible by AirStrip’s technology: A patient has a heart attack and about 15 minutes later, an ambulance that uses AirStrip’s technology arrives. A paramedic immediately takes an EKG, which is sent within seconds to the cardiologist at a hospital and the emergency department. Alternately, the EKG could be sent to a call center for preliminary diagnosis of the patient’s problem and determine which hospital in the vicinity is best equipped to handle it. “Already you are triaging and figuring out which place you are supposed to go, based on the patient’s condition,” Portela says. “This is done by a specialist that is either on call at the hospital’s emergency department or at a call center.” In the end, the patient gets to the cath lab in about 35 minutes.
AirStrip has also observed that the recovery time for such patients is faster. “For patients with a STEMI, we started seeing a decrease in the length of stay in the ICU by 0.85 days—almost a full day,” Portela says. “When our statisticians found out about this, they came to us and they said, ‘Why do you think this is happening?' It is very simple: For these patients, there is less time for the heart to be damaged. If you have a complete blockage to the heart, if you clear that artery in 35 minutes instead of two hours, there is going to be less damage to the heart.”
While activating the cath lab can be life-saving for many patients, a false cath lab activation is expensive, costing roughly $7500. “Somebody will have to pay for that, and believe me, it is not the payer,” Portela says. Because AirStrip technology can help diagnose problems before the patient arrives at the hospital, it can drastically reduce false cath lab activations.
Returning to the case of patients who have suffered a STEMI, following treatment in the cath lab, they will typically spend a few days in the ICU. Then, a patient is sent to a step down area, and a doctor on staff will sign off when a patient is ready to go home. “What happens today is that approximately 7% of those patients who are going home had some dysrhythmia that was not detected by the doctors,” Portela says. “For those people, the odds are that they will come back to the hospital less than 30 days after discharge.” This is a concern for hospitals, which, as a result of healthcare reform, will be financially penalized for such readmissions.
AirStrip technology can address this problem by improving the cardiologists' ability to diagnose problematic EKGs while patients are in the step-down unit following the ICU. “Keep in mind that cardiologists are mobile professionals, and they typically don’t spend much time in the step-down area,” Portela says. “They can, however, analyze those patients’ EKGs on an iPad or a smartphone. Immediately, they can detect that there is a dysrhythmia. At that point, they will order additional studies to see what is happening. They will also look at previous EKGs and [determine] whether this was a condition that existed before or is it something that happened after the heart attack.” If a cardiologist doesn't respond to critical EKG data after a chosen interval, the system sends the data to another cardiologist.
|
To get a better understanding of how the technology affects clinical outcomes, Scripps Health chief academic officer Eric Topol, MD, is planning to lead a clinical trial of the company’s technology. The study, which is still in the planning stages, will be conducted at a large hospital chain over 12 hospitals in Texas. “We are going to be using randomized physicians and intensive care units to see whether continual monitoring to a physician's tablet or phone promotes better outcomes for patients in the ICU,” Topol says.
Intellectual Property Considerations
In August 2012, AirStrip Technologies received U.S. patent protection for technology used to transmit physiologic data natively to mobile devices (U.S. Patent No. 8,255,238). In October, the company filed a suit against mVisum (Camden, NJ), alleging that the patent had been infringed.
AirStrip’s president and CMO, Cameron Powell, MD, was quoted in MobiHealthNews as saying that the patent covers “taking any type of physiologic data—whether that’s from a sensor in the shoe, a home monitor, a blood pressure cuff, or a monitor in the hospital—and then re-rendering it on a native . . . application on a mobile device.”
“[AirStrip’s software] architecture is based on a centralized collection device within the hospital, then transmission of the information to mobile users,” says Bill Betten, medical technology director at UBM TechInsights and a member of MD+DI’s editorial advisory board. “The patent claims information associated with obstetric information, specifically contraction rates and fetal heart rates, as well as limited physiological parameters such as heart rate
and respiration rate.”
The patent could prove to be valuable. The global market for remote monitoring services exceeded $29 billion in 2011, according to IMS Research. Unsurprisingly, a growing number of companies are interested in entering the field. AirStrip’s patent, however, covers transmitting native diagnostic-quality data and appending notes to it, Portela says, while Citrix-based approaches accomplish neither of those objectives.
Speaking broadly of the company’s patent strategy, Portela says AirStrip wants to preserve the quality of care for mobile technology. “We are witnessing the beginning of the whole mobile mHealth industry,” he says. “The last thing we want is for vendors to take shortcuts.”
|
A mockup showing a patient dashboard from AirStrip Technologies. |
Looking to the Future
“We have had a hospital-centric approach to healthcare for the last 20 years,” Portela says, adding that the approach is gradually changing to a patient-centric approach. Ultimately, preacute care will become a greater focus and with it will come more home monitoring.
There are 133 million people in the United States suffering from at least one chronic disease. The cost of addressing chronic diseases is projected to grow, from $1.3 trillion in 2007 to $4.2 trillion dollars by 2023, based on a study from the Milken Institute.
Remote monitoring technology could be used to address this problem. Payers could create a new reimbursement framework that enables healthcare organizations to hire mobile-enabled case managers. “The impact that we can have in healthcare and the economy in the nation is huge. We are about to start the biggest [healthcare] transformation ever,” Portela says.
Brian Buntz is the editor-at-large at UBM Canon's medical group. Follow him on Twitter at @brian_buntz.
You May Also Like