I've Got Surgical Robots on My Mind!
Dr. Gregory Fischer talks about the surgical robotics landscape and gives a preview of the keynote he is set to deliver at BIOMEDevice Boston, later this month.
September 7, 2023

As a researcher, professor, lead investigator on federal government-supported grants, director of a state-funded Medtech accelerator, and founder of multiple medical device companies, Dr. Gregory Fischer has a unique perspective on what it takes to leverage all of the resources to develop meaningful and successful medical devices. Fischer will be a keynote at BIOMEDevice Boston. But before he delivers his speech, titled, "From Concept to Commercialization: It’s not brain surgery, or is it," he joins Let's Talk Medtech for a discussion about surgical robotics.
Here is a transcript of the episode:
Omar: Hello and welcome to Let's Talk Medtech. Thanks for being on the program.
Dr. Fischer: Well, thank you so much for having me.
Omar: I want to jump all in and discuss BIOMEDevice Boston. But first, let's talk a little bit about medical robotics. And let's set the tone a bit for this. Right, so you founded the company, and I just want to talk a bit about how that came to be.
Dr. Fischer: Sure, well AiM Medical Robotics is really the culmination of a ton of very exciting work over the last 15 plus years. Prior to taking the role as CEO of a medical robotics, I've been a professor at Worcester Polytechnic Institute just outside of Boston, and the focus of my research group has been interventional MRI coupled with robotics so that we can do, in engineering terms, closed loop medicine. Right. The whole idea is, as you're doing an intervention, we want to be able to watch the medical images. We want to watch the anatomical targets which may move during a procedure. We want to watch the instruments as they're going in and make sure that we actually hit those targets.
And then if you're delivering a therapy or taking a tissue sample, that you did so in exactly the way that you anticipated. So, over the last 15 years, we've actually had several large NIH R Zero One grants totaling a total of about $15 million with various different collaborators, some in the Boston area and some outside of it, really, to develop this technology. And then Amedical Robotics was founded in 2018, and we've exclusively licensed all the technology that we developed under these research grants into the company. And now what we're trying to do is bring to market these MRI compatible surgical robots. And the primary application that we're targeting right now is Neurosurgery because it's a really exciting area where there's a tremendous need to make sure you get super, super high precision. And unfortunately, a lot of the systems that are out there today, you have really nice preoperative MRI.
You do all of your planning on this preoperative MRI, do your targeting based off of the cranium. Unfortunately, what can happen is tissue inside of the brain, just like any other soft tissue inside your body, can shift and move due to a number of different factors. If that happens, you really don't have a way interoperably to typically know what happened there. So, the idea is that we want to be able to put a robotic device, and when we're talking a robot device, very compact systems inside of the MRI scanner use that real-time imaging to see those changes during the procedure and then update that plan as we go along.
Omar: What about the size of the technology? Just curious. Can you give some more color to it and kind of describe how it works?
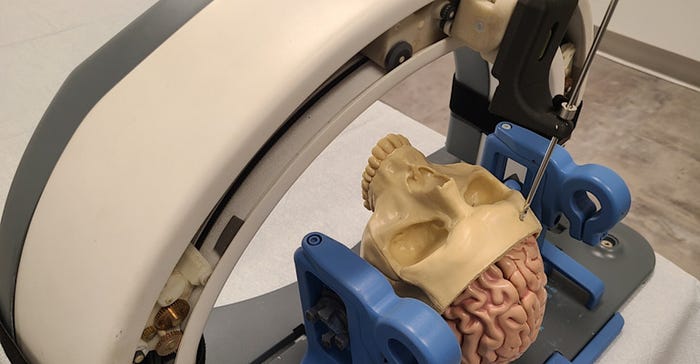
Dr. Fischer: Absolutely. When you think of surgical robotics, or when most people think of surgical robotics, they're thinking really large rated systems doing minimal laparoscopic type surgery. Right. So, you think of something like a DA Vinci or one of the other systems. It's really along those lines. We're not looking for teleoperated systems that have a huge surgeon side console and a huge patient side console. We're also not looking at essentially cart like robot industrial robot arm and then some custom instrumentation on the end of it. We, from the ground up, have developed a very compact, application-specific robot. And specifically, it's effectively an actuated version of a stereotactic frame. Pretty much since the beginning of neurosurgery, there's been metal frames that get bolted on head, and you dial in these different coordinates. And effectively, this is what the large majority of procedures are still done using today when they do stereotactic neurosurgery, despite all of the robotics that are already starting to penetrate the market.
So, what we're trying to do is maintain that workflow that surgeons are very, very comfortable with, but use an actuated version of this stereotactic frame. So instead of going in your navigation software or planning software, identifying these desired coordinates and then taking a screwdriver and manually adjusting this big metal frame and leaving open the problems for human error and all sorts of other issues, we want to streamline that process of going directly from the surgical navigation software to automatically aligning the robot. That also allows the robot to the way and move back again very consistently and repeatedly, which is important since there are steps during the procedure, such as, for example, Draping or drilling burr holes or putting clips in where you really want the maximum access, but then you might need to have your trajectory guide come back again. So, the robot looks a lot like a traditional stereotactic frame, but it's made out of engineering grade plastics, designed in a way to be very rigid, and it's actuated, meaning that we can move this guide around autonomously to the location or the alignment that you want to have. And on top of that, we designed it out of materials and sensors and actuators that allow it to go inside of the MRI scanner.
So, we can use a robot in the traditional operating room setting, where it effectively acts like a robotic stereotactic frame. But once we go inside the MRI scanner, we actually can iteratively take live images from the patient using the MRI to determine the target anatomy, move so we can register the robot to the patient. And then we can take this frame, which, again, is just a small arc-like frame that goes over the patient's head, align it to the trajectory you want. We can drill the bur hole where you think it needs to go.
Then we can take another image. And if there's been shift due to, for example, cerebral spinal fluid loss or swelling or air getting in the brain or just the patient being in a different orientation, we can then take another image and update that trajectory before you actually deliver. Let's say it's a deep brain stimulation lead or a biopsy needle or a precision or. We're also looking into cancer applications where we have needle-based ablation to burn brain tumors. And again, all of these, you want to make sure you hit the right soft tissue. Anatomical targets within the brain not necessarily coordinate relative to the skull.
And then the other real big advantage of this is when you start going into multiple targets. So, for example, deep brain stimulation for Parkinson's is typically bilateral, which means you insert two different electrodes. So, we really want to streamline this workflow in such a way that we can very effectively hit multiple insertions. And then also iterative imaging allows us more accurate on the second and further insertions because we can take image updates because just like any other part of your body, the brain is going to swell, and things are going to move. And if you don't take that into account, you can have reduced accuracy. Again, it's really this compact looks like a little arc frame that goes over the patient's head, nothing like these large gantry or cart like robots. And it can fit right inside the bore of the MRI scanner. So, we can integrate real time imaging.
Omar: So, it doesn't take up that much real estate. There's not that much maintenance when you compare it to other surgical robotic systems. Like Da Vinci.
Dr. Fischer: Exactly. And the whole is that we can just set it up and very quickly put it into a scanner room. So, we had a previous generation version of this robot. Under some of the grant funding that I mentioned previously, we actually ran a 30-patient clinical trial at the Brigham and Women's Hospital here in Boston. And in that scenario, we had the robot essentially from being in a case, buried in a closet in the MRI scanner room on the bed, ready for the patient in under 30 minutes. Which is really pretty tremendous considering some of the other systems that are out there can take one to 2 hours to set up and require an entourage of engineers or at least a technician to fly out and set us up.
Really this idea of having a very streamlined workflow of a very compact device that's very easy to set up in clinical staff. And then the other really important distinguishing feature is that we're not built into a room. So, by not being a very large system or requiring custom penetration panels into the MRI room, for example, or requiring dedicated real estate in in the operating room or the MRI room, we can set this up in any MRI suite, a diagnostic suite or a dedicated interventional suite or an operating room and essentially just wheel it in, set it up and take it out again. There's nothing that requires customization of any of the rooms.
Omar: Now I want to change focus for a bit and I want to talk about BioMed device. Boston, you're keynoting this and I'm going to tell you I was intrigued by the title of the keynote from Concept to commercialization. It's not Brain surgery or is it? Break this down for me, talk a little bit about the title and can you tease the keynote just a bit? We don't want to give too much away, but can you just tease it a bit?
Dr. Fischer: Yeah, of course. So, one of the things that I thought I'd have a little bit of fun here with this is that there's tremendous amount of guidance on there on how to do medical devices. And you can look at tons of books and flowcharts and courses of how can you go from a concept to a commercialization? But it's all very generic, it's not specific to a particular domain or a particular device. And one of the things that we've really noticed as we go along is you need to be able to put yourself in the shoes of the user of the clinician. You almost need to be, in this case, a neurosurgeon, a brain surgeon. Right. I've watched so many of these procedures and I need to understand what are they thinking at each step along the way. It's not about just coming up with this cool idea and how do I get it through appropriate design controls and through it through FDA.
The real hard part about is you need to actually effectively be a brain surgeon or at least think like one and really understand what are these problems and what are these challenges and solve those actual issues and if you want to be successful. So that's what I was trying to get out of this idea, that it's not about just going from how do you go through the steps of the chain to get through the regulatory process and get it commercialized. It's how do you actually do that in a way to solve real world problems?
Omar: Interesting. We talk about the patient journey, right, being a focus of your work. And in this industry, I sometimes feel as if the patient isn't fully taken into consideration sometimes. Can you discuss the patient, the importance of the patient journey and talk about the pitfalls of omitting it?
Dr. Fischer: Yeah, absolutely. And need to look at the big picture. And that's one of the things that's very important. So, if you look at particular procedure, there might be a number you can do it, but you need to think, like, what did it take them to get ready? What's the procedure like itself? And then what happens afterwards? So, if you're going to do a procedure and maybe you can do this procedure invasively, but it has a rate of either recurrence where you have to go back and do a reoperation, or a certain rate of procedures where the target just was not hit right. And you need to go back and do a revision operation, for example. That's hugely impactful on the patient. So one of the goals that we have is we want to make sure we do these procedures right the first time, every time there and that sounds obvious, but there's a lot of cases where that's not necessarily true.
And to me, this idea of using real time interventional imaging is kind of the Holy Grail, because you can guarantee you actually do what you think you're doing during a procedure, as opposed to using what I would almost call stale images of preoperative MRI. And then you might have intraoperative DT or ultrasound, but that's really not the same. And even if you try to do these fusion techniques, that's still synthetic images that aren't necessarily representative. So we want to do things that make sure you do this procedure right. So you can avoid this chance of, for example, having to do a revision operation because your deep brain stimulation leads for Parkinson's didn't go in exactly the right spot and you're not getting the effective units you want. Or maybe side effect. If it's a brain cancer application, we want to make sure you get the best possible margins that match the tumor shape as well as possible, because if you don't, one, they're going to have to go back for another procedure, or the tumor really just is handled effectively. Or two, if you take an over conservative approach, you're going to have tremendous side effects, especially when it comes to brain cancer. It's not like in breast cancer or liver, where you can just take a little bit larger margin in most cases, and that's safe, right? When you're doing brain cancer therapy, suddenly you could affect somebody's memory or their speech or their ability to walk.
So, you need to be super precise. So that's one side of it is just making sure we do these procedures right. So, it's a huge step for them to go and do these surgeries, the last thing you want them to do is have to go again after we've gone through all of this. The other side of it is we want to make this surgery itself as atraumatic as possible for the patient. And a lot of these cases are actually done since they really don't have a great way to guarantee that you're in exactly the right spot, they will do what I'll use, for lack of a better word. Surgeons might not agree with this is essentially various different hacks to make sure you're in the right spot. So, they will, for example, use microde electrode recordings to listen to the electrical activity that you're in the right spot. For example, that means the patient needs to be awake. Typically, often the anesthesiologist will actually wake up the patient and ask them to have some sort of interaction to make sure that they're doing it correctly.
Or they might hook up the electrodes for a Parkinson's case and actually try to see did the tremor get reduced. That's a way to make sure that it's actually working the way you think it should be working before you leave that procedure. But the real reason that you need that is because you didn't have a way to look at the images and guarantee that you were at the right spot. So, by using robot, for example, coupled with real time MRI imaging, we can do these procedures while the patient is asleep, the entire procedure, the procedure time can be cut probably about in half is our estimate. So, it's going to be a faster procedure, a less traumatic procedure, less time under anesthesia, and more importantly, they don't need to be awake during this procedure. They essentially will wake up and their leads are already placed and they're need to be in the right spot. We looked at the images and within the pixel resolution of the MRI scanner, which was used for the original planning in the first place, we can guarantee you're in the right spot.
So, I think that's really a tremendous part of this is that we can make the procedure less traumatic in the first place and then also reduce the chances that they're going to have to go back again and again for repeat procedures. And even when we were dealing with the prostate robot in a lot of our research settings earlier on, which used the same platform, all this technology related to putting robots inside the MRI scanner, I'd say 80% of that is consistent between different devices. The controller is the same, the sensors, the architecture, the wiring, it's just what the end effector essentially, or the manipulator looks like in there. Rather than taking having somebody go and get ultrasound biopsies where they take between ten to 20 biopsies in almost random fashion, if we go in, we can pick the one, two, three lesions that look suspicious in MRI and take biopsies from those specific spots. And what that means is suddenly you can do fewer needle sticks, so that's a big advantage to anybody. But almost more importantly, you have much higher sensitivity so you can get away with less needle insertions and still have a higher percentage chance of actually finding it if something is wrong because you don't want to find out that you have cancer. But if you have it, you better find that sooner than later because you're going to have a better chance of having good outcomes. So again, I think that's a kind of a common thread of let's do these procedures and get the best precision that we can to make sure that we don't have to go back and do that again and do it in as less traumatic a way as possible.
Omar: I think that's very interesting overall, that there's so much consideration for the patient in the patient state of mind, so it's not traumatic for them. And that's refreshing coming from a startup, because I know some companies, they just fall in love with the technology and it's not because they're not trying to help anyone, that's quite the opposite. But they just become so married to how well the technology will work that they don't look at the patient's well-being. Overall, of course, they care about safety and efficacy in all the regulations, but just to take that kind of care, that personal touch for a patient, I think that says a lot.
Dr. Fischer: Thank you so much, I appreciate that. And yeah, I think it's super critical. And again, this also gets back to finding what the real problems and the real challenges are. And I talked before about the challenges for the surgeon, but there's also challenges related to just the whole logistics of the procedure itself, to the hospital, to the patient. And these are all really important things to really understand and consider. And also why I'd really highly encourage anybody to get the opportunity to really watch these procedures, but not just the procedure. Really understand that entire process of how did the diagnosis happen, what happens in between, how did they prep for the surgery, what's actually happening during the procedure and afterwards. Because sometimes it's very easy to think about a quick procedure. A good example would be I had a family member that needed a pretty simple surgical procedure, said, oh, this is a quick five-to-10-minute procedure. I do these all the time. Except the recovery from that procedure was a couple of months, right? So, it's one of those things that it's a pretty straightforward procedure. It pretty much goes well every single time, but you might not be able to walk on that foot, for example, for a couple of months after that. And that's not necessarily thought about the same way. So, it's really important to just really understand all these different parts of the flow, if you will.
Omar: Yeah, I'm going to bring up this is my personal story and we see this in diagnostics all the time. I remember I had to have a physical a few years back and my white blood cell count was low. They didn't have an accurate count for me yet, they hadn't established a baseline and mine was a little bit lower than normal. I just come off being really sick and I remember going through a ton of tests. Some were for cancer, some were for HIV. But what got me was just waiting for the answer, right? Just that time period where I had to wait and it took maybe a few days. And I'm like living in agony. I'm saying, oh my gosh, what do I have? Do I have cancer? Do I have this? It turned out it was nothing.
That was just my established, they just had to establish my white blood cell count. But it's physicians and it's also just medtech companies and diagnostic companies really building in the education to create these products and these devices in the wherewithal to really make it comforting for the patient. Quick results are good, but also just making the patient feel as comfortable as possible and educating them about these procedures. That might take a little bit of time, but it'll take you a lot of time to recover just giving that information. So, I know I went off on a tangent there, but that hit home with me for a bit because it's always this end result in waiting and it almost feels like sticker shock when you get treatment sometimes.
Dr. Fischer: Oh, for sure, that's really good point there. But I would make sure that all the manufacturers and the clinicians when they're working with patients, setting the expectations is important, right? I mean, I think everybody really needs to know what it is that they're getting into. And then there's obviously the other side of this of trying to get as the feedback that we can as quickly as we can, which again, I think when we start using interventional imaging and more broadly than that, there's lots of different means of interventional imaging and also even taking tissue samples and doing analysis on the fly. I think a lot of these interoperative means of getting really meaningful feedback are going to be super transformational because we get that information right when you need it, as opposed to having sent something to a lab and have to wait for a while to find out, did you get the right margins?
As it stands right now, a lot of times they'll cut out a tumor, for example, they'll resect it, they'll send it to the lab and then they'll actually try to figure out did you actually get the margins that you wanted to have? And that comes back in a lab report. If there was a way to on the fly, whether it's using medical imaging or using other types of really cool sensors that are out there now, interoperatively to try to identify where those boundaries are, you'll kind of get that level of confidence much, much faster. In fact, by the time you leave the operating room, you are confident that everything went the way you wanted it to go.
Omar: Yeah. Well, let's talk now. Let's switch focus again and let's talk a little bit about the field of robotics. And surgical robotics has grown tremendously in the last few years, and we're starting to think of surgical robotics more than just Intuitive Surgical’s Da vinci. Right. That used to be the iPhone of surgical robotics, but there's so many different disciplines now. I'm wondering, where do you see the field going in the next few years and what are some predictions that you have for the space?
Dr. Fischer: Yeah, that's a very good question. I used to think of robots, and a lot of people used to think of robots in really two different classifications. There were these teleoperated systems where you could almost think of them as fancy remote control cars or planes, where you have a surgeon console that you move around, and then there's some dexterous manipulators inside of the body. And then there were other devices that were more on the image guided side of things, where you take images and they're almost point and click type surgery devices. You pick a trajectory, you align the target, and then the robot automatically does some sort of just alignment, typically of a straight, rigid instrument. Right. And there are a few other classes, but I would generally think of these image guides and then these tele. What we're starting to see is really this merging of these different types of devices. More imaging and more and more feedback and more and more intelligence is actually being used in these procedures. Moving forward, I would anticipate even a lot of these dexterous manipulation platforms. It's not going to be just purely leader follower type motions. It's really going to start adding intelligence. In fact, even in the research setting, during my faculty appointment, we did work with a research version of the Da Vinci surgical robot, where we're trying to automate or semi automate certain tasks.
So, you can take the biggest advantage of having four arms on the patient side and only two user inputs on the surgeon side. So, things like automating retraction, if you're doing suturing, automating one of the hands so that it could hand something back to the other hand that's being teleoperated, or for example, automating control of an endoscope so that it learns what the optimal viewpoint is for a certain task of a procedure and then aligning that up. So I think adding the of intelligence and then coupling that with unique imaging techniques, whether it's overlays on endoscopic videos or incorporating ultrasound or incorporating interoperative like MRI, for example, I think the ability to use real time feedback, and I know we have a lot of engineers that are in the audience. Again, I like to use the term closed loop medicine, right. Closing the loop with feedback. And to me, that's one of the ways to see things going. The other direction that I think is going to be really important moving forward is these smaller, more compact, application specific devices. There certainly is and will continue to be a need for very large robots that have generic applicability to a lot of different indications. But I foresee a lot of smaller, lower cost application specific devices for various different anatomies and clinical needs.
And you might get to the point that some of these, you may not even necessarily think of them as robots. Right. These might be just small, automated devices that have some intelligence in them that are helping with a certain aspect of a procedure. And I think there's just going to be more and more growth of these. And quite frankly, I think it's going to be somewhat of a natural progression. And again, some of these you might not as a robot.
Omar: Yeah, it will be interesting to see where we go five to ten years from now. There are definitely a lot more companies, a lot more startups, and a lot more medtech firms playing in the space. We've seen some of the larger strategics make acquisitions to be a part of the surgical robotics ecosphere. So it's really a hot market right now, a hot space that's teeming with activity.
Dr. Fischer: Yeah, absolutely. It's an incredibly exciting field to be in and I'm so excited to have stepped in with both feet to lead a medical robotics because it's just so much going on right now. And I really see huge opportunity for what we're doing, but also just more broadly, how we can come up with really new, cool robotic devices. And I think one of the things to get across is it's not just about the AI and the image processing. That's a huge aspect of it as well. But there is so much opportunity for coming up with cool, new, very useful, clever manipulators control systems, electronics. I mean, this is really an all-hands-on deck effort and I think there's a huge opportunity to be really unique new devices.
Omar: Now I have to go back to because I'm sure Adrienne Zepeda would kill me if I didn't ask this question, but I have to go back to the keynote for a second and I just want to ask if we can bring it back home and talk a little bit about that. Out of all your experience, out of what the company is doing, what are you hoping that attendees will get out of the keynote and will they hear some of what the company is doing, what a medical robotics is doing in the space?
Dr. Fischer: Oh, for sure. I'm very excited to present what we're up to and where we're going and this really unique approach of taking robots and putting them inside the MRI scanner. And from an engineering perspective, I think actually folks will. Find it very interesting because robots are made of steel. They're usually actuated by motors. A motor is what? A steel can, a magnet and a coil wire. Those are probably the three worst things you could MRI scanner. So, it's a really interesting engineering problem that I'm looking forward to talking about. But more broadly than that, I really think emphasizing understanding what are the needs, right? And getting back to what I mentioned earlier, putting yourself in the shoes of the surgeon and not just the surgeon, but also the clinical staff, the nurses that are going to be setting this up, for example, also ending again that patient journey. As we've talked about, it's really important to understand all those players that are involved in the use of the device and really understand what the real challenges are. And we can run through some case studies, if you will, of what we've come across. But I'd say the general point there know really understand what the real problems are from the real users.
Omar: Sounds good. Well, I look forward to hearing the keynote and I'm sure it's going to be an amazing time in Boston.
Dr. Fischer: Absolutely. I'm very excited. Thank you very much.
About the Author(s)
You May Also Like



.png?width=300&auto=webp&quality=80&disable=upscale)
