The Evolution of Robotic Technology: From Robotic Assistance to Augmented Intelligence to Elevate All Surgery
Leveraging artificial intelligence and machine learning in robotic surgery could help surgeons reach more patients, in more care settings, with a greater variety of procedures.
Surgery today is inconsistent. Surgeons of all skill levels, experience, and training perform similar procedures, but they have vastly different outcomes. This lack of standardization directly impacts procedural safety, increases costs, and diminishes the surgical experience for both the patient and surgeon. Too many patients are suffering adverse outcomes and complications following surgery, which can result in increased length of stay, repeat surgery, and additional medical treatment. In fact, one in five surgeries result in one or more complications.1 Moreover, the physical and cognitive demands put on surgeons are strongly associated with musculoskeletal disorders and injuries,2 surgeon burnout, and medical errors.3
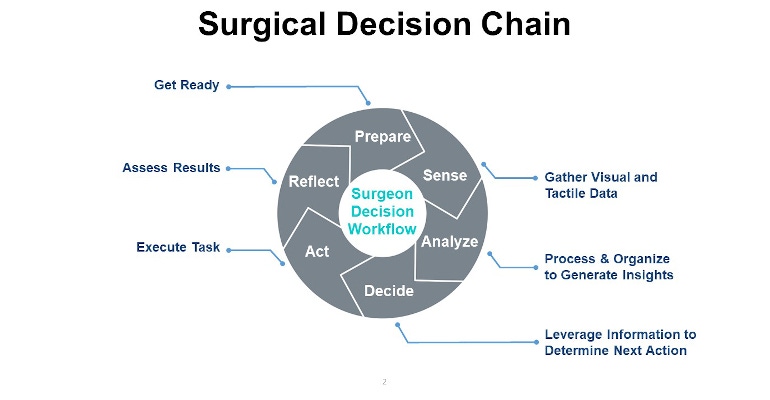
When a surgeon operates, she moves through a surgical decision chain, which is a series of defined steps, thousands of times until the procedure is complete, as shown in the figure above.
Historically, technological innovation in the operating room (OR) has been focused on surgical tools to improve the acting portion of the surgical decision chain during which the surgeon is executing a chosen decision like throwing a suture. However, there has been very little focus on improving the intraoperative, or decision-making aspects of the surgical process, which is crucial in the high-pressure, highly variable situations that drive surgical outcomes. Additionally, little advancement has been done to improve the physical comfort of the surgeons operating on the patients—until now. Using robotic technology, powered by artificial intelligence (AI) and machine learning (ML), operating rooms are being transformed—and in turn so is surgery performance.
Transforming ORs with Technology
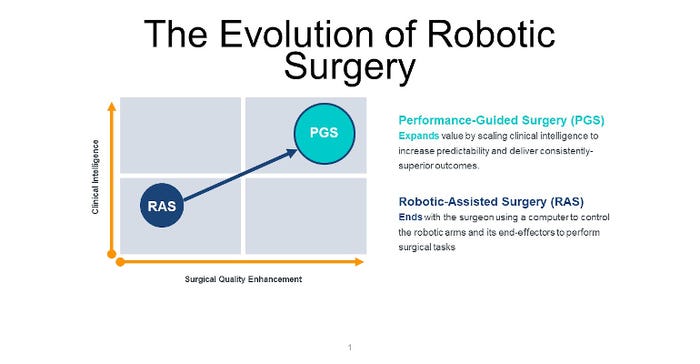
Twenty years ago, robotic-assisted surgery (RAS) that used computer and software technology to control and move surgical instruments through one or more tiny incisions in the patient’s body was introduced. The benefits of robotic surgery are the ability to facilitate minimally invasive surgery and assist with complex tasks in confined areas of the body with more precision, flexibility, and control than is possible with conventional techniques. For patients, this results in smaller incisions, shorter recovery time, and less pain. RAS is currently performed in less than five percent of all surgeries, with the majority (60%) being performed via manual laparoscopy.
In 2017, the interface between the surgeon and patient was digitized (digital laparoscopy) providing the benefits of RAS with expanded control and clinical intelligence while performing laparoscopy. Digital laparoscopy integrates additional technological advances to help surgery become more instinctive, more responsive, and more focused. In return, this creates an environment for surgeons that is more conducive to perform a greater variety of procedures, reach more patients in more care settings, and lessen the physical toll on surgeons.
When AI and ML are added to robotics, all six phases of the Surgical Decision Chain can be addressed, unlocking the clinical intelligence to increase predictability and deliver consistently superior outcomes. Together, these three technologies are enabling a new era of digital surgery called performance-guided surgery (PGS) that mitigates surgical errors and complications—regardless of surgeon knowledge and experience. (See the figure below.)
These advanced digital technologies can enable surgeons to take the best surgical practices and techniques from everywhere and leverage them anywhere to help improve outcomes, reduce variability, control the unexpected, reduce costs, reduce cognitive and physical fatigue of surgeons, and provide patients with optimal care.
Analyzing the Technology that Makes This Evolution Possible
Digital laparoscopy today and the evolution to PGS are made possible by one advancement at the forefront of the surgical industry called augmented intelligence, which focuses on the assistive role of AI, designed to enhance human intelligence, rather than replace it.
In the surgical field, augmented intelligence enables a digital platform to perceive, learn, and assist in surgery—providing a digital surgical assistant for the first time. It can enhance workflows and enable new levels of precision and accuracy to be carried out. This technology can make drastic improvements in the minimally invasive space. Examples include the ability for surgeons to measure a defect before placing mesh, a highly variable and important step in many procedures; as well as eye-tracking camera control to decrease the need for surgeons to work outside the visual field and to keep free the hands of surgical staff for other in-room activities.
Augmented intelligence also helps maintain the personal touch and authenticity innate in healthcare practices and helps in areas where human intelligence can benefit from its assistance. Unlike artificial intelligence, augmented intelligence serves as a “navigation system,” or a “digital twin” that can account for individual patient differences and complications by generating an algorithm based on a range of data from similar surgeries done on similar patients, curating the surgeons��’ experience.
Augmented intelligence technologies, including machine vision and machine learning, will play an increasingly significant role in the healthcare industry. The introduction of these new capabilities represents an important step to dramatically improve critical decision making, driving predictability and helping level-the-field by gathering, analyzing, and presenting rich information and insights to empower surgeons of all levels of experience with deeper situational knowledge.
The Benefits Surgeons Are Seeing
At this moment, there is a lot of excitement around digital laparoscopy. Surgeons are seeing these enhancements first-hand, from a more economical way to use robotics in more surgeries to improved ergonomics and reduced cognitive toll. Digital laparoscopy provides surgeons with a relaxed sitting position, familiar movements based on laparoscopy, an eye tracker to allow surgeons to control the camera for the first time simply using eye movements, haptic force feedback for an increased level of security, a digital fulcrum to create a dynamic virtual pivot point that helps minimize the incision trauma and limit forces applied on the patient, robotic 3-mm instruments to make surgery even less invasive, and the ability to have a direct line of sight to the patient and the OR team for greater efficiency.
As such, many surgeons are performing an increased number and a wider variety of digital laparoscopy procedures. Case in point, Prof. Dr. med. Dietmar Stephan, of St. Marien Hospital, Siegen, Germany has completed almost 400 digital laparoscopies. He started with procedures for inguinal hernias using the TAPP technique, expanded to upper GI operations, including fundoplication and EndoStim implantations, and then proceeded with colorectal surgeries and integrated sigmoid dissections.
By transforming the surgical view in real-time into insightful and actionable data, technology assisted by robotics, machine learning, and augmented intelligence can provide innumerable applications for surgeons to take action on information that was once hidden in plain sight. Armed with this new ability, surgeons can provide the best outcome for every patient, every time. The industry is at the pinnacle of realizing just exactly what performance-guided technology can do for minimally invasive surgery.
References
Eelke Bosma, MD, et al. "Variable impact of complications in general surgery: a prospective cohort study." Can J Surg. 2012 Jun; 55(3): 163–170.
Cima RR, Brown MJ, Hebl JR, et al. "Use of lean and six sigma methodology to improve operating room efficiency in a high-volume tertiary-care academic medical center." J Am Coll Surg. 2011; 213:83-94.
Blendon RJ, DesRoches CM, Brodie M, et al. "Views of practicing physicians and the public on medical errors." N Engl J Med. 2002;347(24):1933-1940.
About the Author(s)
You May Also Like




