Programming Red Blood Cells to Carry Drugs
December 10, 2015
A new startup looks to tackle hard-to-treat genetic disorders and diseases through genetically engineered red blood cells.
Kristopher Sturgis
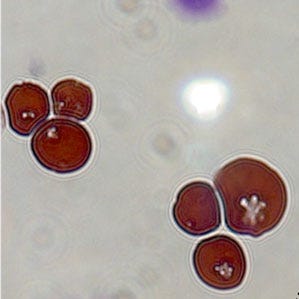 The new technology, unveiled by recent startup Rubius, could serve as a platform for a host of new therapies that carry fewer safety risks. The science behind the technology focuses on turning red blood cells into drug-delivery vehicles, and could serve as a platform for other biological therapies that could be used to treat a range of disorders from hematologic and autoimmune disorders, to infectious diseases and cancer.
The new technology, unveiled by recent startup Rubius, could serve as a platform for a host of new therapies that carry fewer safety risks. The science behind the technology focuses on turning red blood cells into drug-delivery vehicles, and could serve as a platform for other biological therapies that could be used to treat a range of disorders from hematologic and autoimmune disorders, to infectious diseases and cancer.
This latest breakthrough comes off the back of the company's recent work surrounding the ability to genetically modify and grow human red blood cells in culture. That work is what eventually led scientists from Rubius to engineer progenitor cells taken from human bone marrow, and actually grow blood cells that can produce specific therapeutic proteins, either on the surface or inside the cell.
As a therapy, red blood cells become easier to control because they eject their genetic material before they become fully mature, making them less risky than other stem cell or gene therapies. And because human red blood cells circulate for as many as four months, they could serve as a potential basis for long-term therapies. That kind of time provides the cells with the ability to circulate anywhere in the body through the bloodstream, and can protect any therapeutic agent that the immune system tries to reject.
Scientists began testing the technology on phenylketonuria (PKU), a debilitating genetic disorder that can leave patients without the ability to digest the amino acid phenylalanine, something commonly found in high-protein foods. The disorder can lead to a variety of serious health concerns, and can even result in brain damage. The only treatment for the disorder is a very restrictive diet that can have its own complications, and prevent patients from ever finding any real cure.
Of course there are identified enzymes that can break down phenylalanine, but the issue has been finding a way to slip these enzymes into the body undetected by the immune system. The body will quickly clear the enzymes if they are injected directly into the bloodstream, and can even trigger an immune reaction that would render future treatments of the same enzyme useless. This new technology eliminates both risks through the engineering of red blood cells that can produce the desired enzyme, enabling patients to digest phenylalanine naturally.
Harvey Lodish, a professor of biology and bioengineering at MIT told univeristy news that recent animal tests suggest that engineered red blood cells can be a "very potent" therapy for a range of diseases. Lodish, who also serves as scientific cofounder and a member of the board of directors for Rubius, says that some of the work from his lab has shown that cells modified to produce a specific antibody to a bacterial toxin has rendered mice resistant to many times the lethal dose of that toxin.
For now Rubius remains focused on refining the technology as a drug therapy solution for PKU. While the company won't speculate about what additional drug therapies we could see in the future as the technology progresses, the potential for this kind of therapy should be worth keeping an eye on in the coming months.
Learn more about cutting-edge medical devices at MD&M West, February 9-11 at the Anaheim Convention Center in Anaheim, CA. |
Kristopher Sturgis is a contributor to Qmed and MPMN.
Like what you're reading? Subscribe to our daily e-newsletter.
About the Author(s)
You May Also Like


