April 27, 2017
Pediatric researchers design an innovative new fluid-filled device that can mimic the prenatal environment that newborns need for organ development.
Kristopher Sturgis
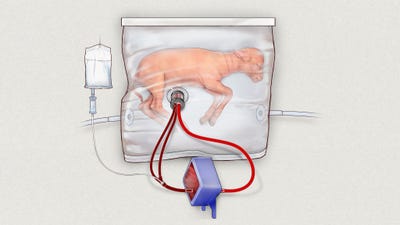
Researchers at the Children's Hospital of Philadelphia are developing a womb-like device that has already been tested on fetal lambs. The system could provide pre-mature infants with a fluid-filled environment to finish developing vital organs.
Pediatric researchers from the Children's Hospital of Philadelphia published a new study this week that details the development of a new technology that aims to reduce the mortality and disability rates in extremely premature babies through the use of a transformative new womb-like device. The device could provide an environment that mimics the womb, where premature infants could finish developing vital organs like the lungs and heart.
The new technology uses a unique fluid-filled container that attaches to machines that have been custom designed to provide physiological support. So far, the system has been successfully tested on fetal lambs, and researchers have observed prenatal lung and organ development of the prenatal lamb test subjects. The study placed fetal lambs in a temperature controlled, near-sterile environment where they could breathe amniotic fluid, just as they do in the womb.
The new technology even allows for the fetal hearts to pump blood through their umbilical cord and into a gas exchange machine outside the bag to provide oxygen. The system also uses electronic monitors to measure vital signs and blood flow, among other physiological functions, to help neonatal physicians monitor their progress.
Recent studies show that roughly one in 10 babies born in the United States are born before 37 weeks -- the standard mark for premature birth -- and about 30,000 are born before 26 weeks, where they are considered critically preterm. These critically premature births account for the leading cause of infant mortality in the United States, totalling one-third of all infant deaths, and also account for roughly half of all cases of cerebral palsy.
Neonatal doctors and pediatric researchers have been exploring various new avenues of treatment to help reduce these mortality and disability rates in premature babies. Last summer, researchers from the University of Michigan created an extracorporeal artificial placenta that successfully saved the lives of five extremely premature lambs. They too have been working toward the development of an artificial intrauterine environment to support critical organ development.
However, this new system is the result of a three-year study that has seen a series of prototypes evolved into a device that can actually mimic life in the uterus as closely as possible, according to the researchers. There is no external pump that drives circulation, no ventilator -- as the infant's lungs are too immature to breathe in atmospheric oxygen -- and the baby's heart would continue to pump blood through the umbilical cord through the system's low-resistance external oxygenator.
The system also uses amniotic fluid produced from a laboratory that can flow in and out of the bag, allowing fetal lungs to function inside the fluid. Simulating this amniotic environment promotes crucial organ development while also supplying the infant with vital nutrients and growth factors. All of this is accomplished in a sealed and sterile environment that can be insulated and protected from hazardous infections.
While similar technologies have been developed in the past, this device is the first of its kind to provide a pumpless system that can operate for up to 28 days while keeping its occupants healthy, according to the researchers. No other system has been able to last more than 60 hours, and this device has enabled extremely premature fetal lambs to show normal maturation of the lungs and vital organs, grow wool, and exhibit natural neurological growth and functionality.
The next step for the group will be to refine the system, and scale it down for human infants, who are roughly one-third the size of fetal infant lambs. The researchers said that if these results translate into human clinical care, the system could be in place within the next decade, and potentially establish a new standard of care for extremely premature infants.
Kristopher Sturgis is a contributor to Qmed.
[Image credit: Children's Hospital of Philadelphia]
About the Author(s)
You May Also Like


