Patient-Centric Human Factors
Medical device manufacturers and their customers are required to implement design standards that incorporate patient-centric human factors, including physical capabilities, learning abilities, and social or emotional context. Failure to address these factors can lead to a host of product-related use errors and strategy failures. In support of successful launches in the patient and home healthcare market, this article presents an overview of human factors and usability testing, including:
Why it is important to test human factors.
Who should be included in the sample and who should conduct the survey.
Where testing should take place.
What things must be tested.
How to approach testing.
Why
Beyond the mechanics of therapy delivery, medical devices need to be designed to be safe and easy to use, and to accommodate a broad range of user capabilities and environments. As the trend of patient-administered therapies for chronic conditions have increased, so too has the need for better requirements. FDA’s Medical Home Use Initiative focuses on patient outcomes and cost-to-benefit ratios. In addition to supporting device approval, correct emphasis on human factors and usability testing allows manufacturers to improve design and avoid the risks associated with the following:
Physicians underprescribing therapy because they underestimate a patient’s ability to use a device.
Patient failure to initiate therapy; poor compliance and adherence.
Incorrect therapy administration.
Poor patient outcomes.
Increased adverse events and recalls.
Potential legal liability for device and drug manufacturers.
To avert such issues, it is crucial to include human factors and usability testing in each phase of device design for these markets.
Who
It is critical to select the appropriate sample for a study. For example, an insulin pen study might include diabetics who currently use a pen but have varying levels of experience (e.g., a patient who recently began using a pen versus a long-term user), as well as those using vials and syringes (potential pen users). User expectations for how devices work differ from those of engineers. In addition, patients use a device in a natural environment that is embedded in a social context, which is very different from an engineer manipulating the device in a lab or healthcare facility. Other respondents for an insulin pen study could be the physician prescribing the device and the diabetes educator instructing the patient. Each of these respondent types provides critical perspectives on the human factors that are involved in device design.
The sample sizes for an in-person qualitative study depends on the objectives; however, it is often recommended to have at least 15 respondents per respondent type. Including a wide range of respondent types is vital to ensuring that the sample encapsulates the typical patient population for the device. Unlike clinical testing, it is not necessary to have a statistically representative sample, but this range should take into consideration age, comorbidities, education level, and experience level with the device. The sample should include patient categories that cover the range of possible users, from most likely users to worst-case-scenario users. The general rule of thumb is that the riskier the effects of misadministration, the more thorough the usability testing needs to be and the more potential users need to be enlisted.
Human factors and usability testing should always be conducted by an independent third-party expert to ensure objective credibility with regulatory agencies and to prevent inadvertently encouraging a specific response bias. It is important to select a market research company with a trained moderator who is experienced in usability testing, human factors, and medical device research. Delegating the market research allows the medical device team to concentrate on the results, including close observation of the respondents’ motions.
Where
Ideally, the testing environment should be similar to the environments where a patient typically uses the product. Often, ethnographic testing in the patient’s home or workplace is not possible, is logistically challenging, or exceeds the project budget. A central facility is often used because it can provide two-way mirrors for live viewing of research, remote viewing through video streaming, or high-quality video and audio recording for later review. It is useful to have R&D engineers, human factors consultants, regulatory specialists, and marketers observe the research.
Having the team on-location means potential adjustments can be made between interviews. When not testing in a respondent’s natural environment, the moderator should set the scene by having respondents visualize where they would use the device, what supplies must be on hand, what are the potential distractions, who might be present during device use, and other concerns. Additionally, it’s important to consider what time of day the device is typically used (e.g., early morning, at work, before bedtime).
|
What
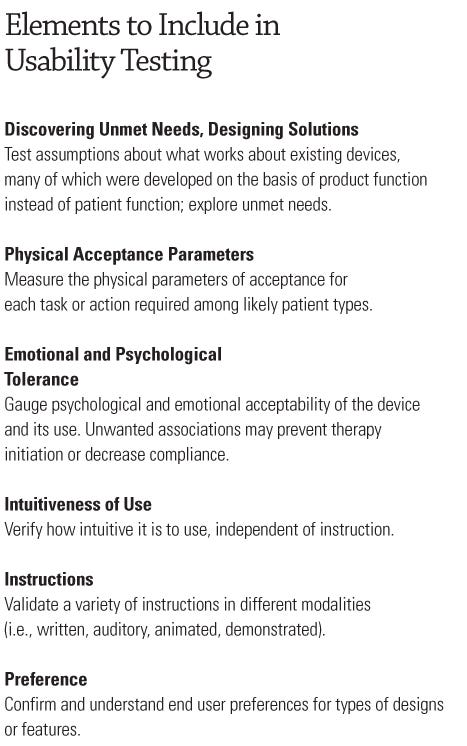
The research methodology used depends upon the research and business objectives (see the sidebar “Elements to Include in Usability Testing” on left). The approach should be customized, rather than rely on standard cookie cutter methods. A few typical study types are briefly reviewed here, including the following:
Discovering unmet needs.
Physical acceptance parameters.
Emotional and psychological tolerance.
Intuitiveness of use.
Instructions.
Preference.
How
Discovering Unmet Needs and Designing Solutions—What’s Missing? This research is designed to find out what doesn’t currently work and where a manufacturer might be able to develop a better, differentiated product by designing a solution to a current hurdle in usability. This discovery phase is best done in qualitative research and in person—either individually or in a small group (no more than five people).
Prototypes or samples of current products are also helpful aids. Users can be probed on initial experiences with the therapy and how they learned to use the device. Each step of the procedure should be broken down into specific tasks. These may include preparation, administration, and cleanup or disposal. For risky tasks (e.g., injections, site preparation), proxies (e.g., prosthetic arm) should be used. Each of these tasks can be analyzed for barriers and drivers for successful completion of the task, which may include concerns about the environmental or social context, required supplies, and psychological or lifestyle factors. Results of the research should include a list of desired device attributes and features as well as potential barriers to use. This information can be used by the R&D engineers to design an innovative device.
Testing Physical Acceptance Parameters: How Far and How Fast? There are a variety of methods to test physical acceptance. One method is to choose a few levels of each attribute to be tested so that the highest level and the lowest level are a priori near the boundaries of what users are expected to perform for the given action. Respondents attempt to perform the task with each level and rate if the level is acceptable (yes or no, or a rating scale). Typically, there is a prototype for each attribute level tested. The advantage of this method is that it works well when there are several attributes that must be tested and time is limited. The disadvantage is the need for a priori boundary levels.
A second method is to have respondents try increasing levels of an attribute until they reach their threshold of considering it unacceptable, or they are incapable of performing the action. Upper and lower threshold boundaries can be attained through psychometric testing using this methodology. The advantages of this method are that a priori boundaries are not needed and the sample size can be smaller. The disadvantages are that the method is time-consuming. Instead of having a prototype for each attribute level, a device needs to be constructed to allow for continuously increasing or decreasing the attribute.
A third method is to directly measure respondents’ physical abilities, such as thumb depression strength or range of motion. The recent HE75:2009, “Human Factors Engineering—Design of Medical Devices,” includes a chapter on anthropometric design parameters for national averages.1 However, because the device being tested is meant to be used by a specific type of patient, national averages will not be as useful as testing a sample of the actual patient type. Regardless of which method is used, once the upper and lower bounds are better understood for the specific patient type, protocols can be used to design products that comfortably meet the optimal range of potential user capabilities.
Testing Emotional and Psychological Tolerance: You Want Me to Do What? If the patient associates the actions of a procedure or the aspects of a device with something that they find inappropriate to their self image, they will likely not comply with their doctor’s recommendation for treatment—even if a device is medically necessary and beneficial to the patient. For example, if a 45-year-old male construction worker thinks his EpiPen or asthma dispenser looks like lipstick or a feminine contraceptive case, he is unlikely to use that device in front of his coworkers, take it to work, or leave it in the communal refrigerator where it must be stored. An expert moderator can uncover psychological associations and social context barriers.
Testing Intuitiveness of Use: How Does This Work? This phase of research is intricate because it requires precise observation for correct analysis. It is critical that video captures every motion and that the audio quality is high enough to capture auditory feedback from the device. With no instructions, patients are asked to employ the device the way in which they think it should work. Every hesitation, incorrect motion, and error is recorded, and the patient is questioned regarding what would make the task easier to complete. In aggregate, the observations are reviewed to determine the best and easiest set of steps to complete the procedure. This must be done with in-person individual interviews, and a human factors engineer should be actively observing the test or the recorded results.
Testing Instructions: What Does This Mean? In this phase of research, the instructions accompanying the device are tested. Instructions need to accommodate different learning styles and cognitive capabilities, as well as provide alternatives for degrees of hearing or visual impairment. If the device is accompanied by video, training, pictures, or written instructions, all of these need to be tested to make sure that they are comprehensive and comprehensible. The critical situation to avoid is when a patient is in the middle of a task, unsure if it is complete, and confused about the next step. This research must be done with individual in-person interviews to ensure that after instruction, the patient can complete the task correctly and knows the task is finished. These tests should be carefully observed and diligently recorded, and may be part of FDA submission protocols.
Preference. In an acceptance study, respondents decide whether an attribute or attribute level is acceptable in the use of the product. In a preference study, respondents choose between designs or attributes. This study often follows the unmet needs study to reduce the number of new features that are integrated into an existing device in its next generation or to shape the basic design of a completely new product. This type of research can be done with focus groups in which respondents interact and discuss the reasons for their choices. It can also be done with individual in-person interviews, which allows for more in-depth probes and understanding of an individual’s preference without interference of another’s opinion.
Conclusion
Incorporating usability testing into device design contributes to a company’s ability to address patient needs, ensure positive patient outcomes and safe use, and encourage therapeutic compliance. Although there are many steps involved in ensuring that device design can achieve these goals for the home healthcare and self-administered sector of the market, the payoff is a successful product, less manufacturer liability, lower healthcare costs associated with medical errors, and healthier users. An expert research consultant with device testing experience can support usability testing and a product’s optimal configuration and success.
Reference
1. ANSI/AAMI HE75:2009, “Human Factors Engineering—Design of Medical Devices,” (Arlington, VA: Association for the Advancement of Medical Instrumentation, 2010).
Rebekkah Carney is vice president of MedTech Market Research at Double Helix USA (Fort Washington, PA). Tom Donnelly, PhD, is associate director of market research at the firm.
About the Author(s)
You May Also Like