Titanium Nanotubes Offer Implant Integration, Drug Delivery
May 17, 2009
Originally Published MPMN May 2009
NEED TO KNOW
Titanium Nanotubes Offer Implant Integration, Drug Delivery
|
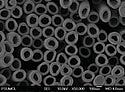
A research team has developed a bottom-up process for growing titanium nanotubes on implants. |
When it comes to nanomedicine, researchers are racing to unlock the secrets of carbon nanotubes. A research team out of Colorado State University (CSU; Fort Collins, CO; www.engr.colostate.edu), however, has strayed from the pack, choosing instead to explore the potential of titanium at the nanoscale. As it turns out, going off the beaten path has paid off. The CSU researchers, along with partners at The Pennsylvania State University (University Park, PA; www.psu.edu), have discovered nontoxic titanium nanotubes that they believe are brimming with the potential to promote biointegration of implants and provide local drug delivery.
Led by Ketul Popat, an assistant professor in the department of mechanical engineering at CSU's school of biomedical engineering, the research team has developed a bottom-up process that, when applied to a titanium implant surface, yields growth of titanium nanotubes. These nanostructures could help to significantly extend life and facilitate integration of permanent titanium orthopedic implants for knees and hips, for example. "By putting these nanotubes on titanium, we found that bone tissue is interacting much better than it ordinarily does with the smooth surface," Popat says. He speculates that improved integration could be attributed to the more-similar geometry of the nanotube array to natural tissue on the nanoscale.
No coatings or additives of any sort are involved in the nanotube growth process, Popat stresses. Simply put, the 3-D, nonplanar shape of most titanium orthopedic implant surfaces, when treated, is conducive to growth of nanotubes from the source material. And, because titanium nanotubes retain the same properties as the bulk material, they are biocompatible, stable, and do not introduce any new or unexpected problems. "We're not adding a new material to the implant," Popat explains. "Titanium has a native oxide layer. We're just taking that native oxide layer, changing it, and making it into nanotubes."
The growth process, when altered, can produce nanotubes in a variety of sizes. This capability is advantageous, Popat says, because it opens up the possibility of also employing the nanotubes for targeted drug delivery. "Since we can control the size of the nanotubes, we can control how much drug is coming out and how fast it's coming out."
Currently producible with diameters ranging from 20 to 200 nm and in lengths from 200 nm to 20 µm, the titanium nanotubes could be used to locally deliver antibiotics at the implant site to prevent infection. They also hold promise for use on stents and possibly even for cancer treatment. Popat points to the example of osteosarcoma, a type of bone cancer that often requires an implant upon removal of a tumor. He hypothesizes that someday patients might benefit from targeted, in-body delivery of chemotherapy via the nanotubes, which would eliminate the need for postoperative treatments and their associated side effects. Although such applications are not realities yet, the researchers predict that the technology may be ready for commercialization within the next two to three years.
Copyright ©2009 Medical Product Manufacturing News
You May Also Like