Best of Both Worlds: SOPs for Device Trials In Europe, Part 2
Navigating device clinical trials in Europe may require creating a hybrid procedure that uses both ISO 14155 and the ICH-GCPs.
July 1, 2007
CLINICAL TRIALS
|
Illustration by Taisha Payton |
When device manufacturers get ready to conduct clinical trials, they often look toward Europe. In general, European trials can be easier, and results can be gathered more quickly than in the United States. Conducting European trials can be tricky, though. European regulators recognize both ISO 14155, “Clinical Investigation of Medical Devices for Human Subjects—Parts 1 and 2,” and the ICH-GCPs, The International Conference on Harmonization—Good Clinical Practices (document number E6).1,2
For device manufacturers who decide to conduct their first-in-human trials in Europe, the question of which document to follow can be a difficult one. Following the ISO 14155 is easier and will bring the device to market in Europe faster, but the data may be of limited value in the United States. Following the ICH-GCPs in Europe is more burdensome but more likely to result in data that are usable in the United States. The best method of conducting trials is to use neither ISO 14155 nor the ICH-GCPs, but to create a composite guidance. By using both documents to create a unique set of standard operating procedures (SOPs), device makers can satisfy the requirements for conducting trials in Europe and in the United States.
This two-part article reviews the eight sections of the ICH-GCPs and compares them with ISO 14155. Through the comparison, a device OEM can determine whether the ICH document is relevant to its medical device trial needs. Part 1 of this article, published in the May issue of MD&DI, reviewed the first four sections of the ICH-GCPs.
This second part looks specifically at Sections 5–8 of the ICH-GCPs. Subsections are skipped when they are consistent with standard medical device practices. Recommendations for preparing corporate SOPs follow each Item.
Section 5. This section of the ICH-GCPs covers sponsors' accountability. The document states that the sponsor is responsible for implementing and maintaining quality assurance and quality control systems with written SOPs. This requirement is to ensure that trials are conducted and data are generated, recorded, and reported in compliance with the protocol, GCP guidance, and applicable regulatory requirements (5.1.1–5.1.4). The ISO document says only that “The sponsor shall ensure [compliance] through a quality system,” without giving detail as to what that system should include (Part 1-8.1).
Item. According to the ICH-GCPs, a sponsor may transfer any or all of the sponsor's trial-related duties and functions to a contract research organization (CRO), but the ultimate responsibility for the quality and integrity of the trial data always resides with the sponsor (5.2.1–5.2.3). ISO mentions CROs only in passing, as an example of an additional party to be listed in the final report (Part 1-C.13.c). This is in spite of the fact that delegation to CROs frequently occurs in the device industry.
Recommendation. An OEM's quality system should take both guidances into account. It should specifically address CROs when applicable.
Item. The ICH-GCPs provide for the establishment of an independent data-monitoring committee (e.g., a data-safety-monitoring committee in the United States) (5.5.2). They mention several items regarding electronic data handling (5.5.3) and specify that an original copy of data should be archived before it is transformed during processing (5.5.4). In addition, the guidance mentions the possibility that the sponsor may not be the owner of the data (5.5.6) and discusses the transfer of ownership of data (5.5.10). It states that data should be retained for a period of two years (5.5.8). None of these elements are discussed in any detail in ISO 14155.
Recommendation. Follow the data-monitoring requirements set forth by the ICH-GCPs in your corporate quality system.
Item. ICH asks for an agreement between sponsor and investigator for financial aspects (5.9). ICH's approach to agreements is different from ISO. ICH allows the protocol to substitute for an agreement between sponsor and investigator. It also suggests a second agreement on financial matters. ISO requires a unique, written agreement between sponsor and investigator and is silent on financial matters.
Recommendation. The issue usually shakes out as a result of institutional policy at the investigative site. Any site with experience requires a financial agreement. Although some sponsors combine trial and financial matters into one agreement, it may be unwise to do so because financial documents can be complex. The investigator should personally sign an investigator agreement; a financial manager at the site should sign the financial agreement.
Item. The section in the ICH-GCPs on manufacturing, packaging, labeling, and coding reveals a fundamental difference in drug thinking versus device thinking. In the ICH-GCPs, an investigational product must be “manufactured in accordance with any applicable GMP” (5.13.1). ISO takes a different strategy. It requires an investigator's brochure that provides a literature summary, a list of materials and components, the intended clinical performance, a summary of relevant preclinical data, and a summary of previous clinical experience. In addition, ISO states that investigators must provide a list of international standards complied with and results of the risk analysis (Part 1-7.2). These data are intended to support the safety and appropriateness of the investigational device and substitute for compliance with good manufacturing practices.
Recommendation. FDA guidelines, 21 CFR Part 812, take an approach similar to the ISO standard. FDA asks for a report of prior investigations and a statement as to the extent of compliance with good manufacturing practices. Because clinical trials in Europe are often a stepping stone to gaining approval in the United States, it makes sense to follow the ISO standard.
Item. ICH-GCP says sponsors should ensure that monitors, auditors, institutional review boards (IRBs), and regulators have direct access to source data and other trial documents. Such an agreement must be in writing, and sponsors should verify that subjects have consented to such access (5.15). ISO only mentions data access indirectly and with much less emphasis.
Recommendation. Clearly, giving direct access is important to the success of a clinical trial. The written agreement should be incorporated into the sponsor's contracts and procedures.
Item. The ICH-GCPs state that the sponsor should expedite the reporting of all serious and unexpected adverse drug reactions (i.e., adverse device effects) to other investigators, other IRBs, and to regulators (5.16.2). ISO 14155 is broader than the ICH-GCPs. ISO requires sponsors to report all serious adverse device effects and all other serious adverse events to regulators, ethics committees, and safety-monitoring committees, and to other principal investigators (Part 1-8.2.h and Part 1-8.2.i).
ISO 14155-1, section 3.19, defines a serious adverse event as one that leads to a death or a serious deterioration of health, or leads to fetal distress, fetal death, or birth defect. A serious deterioration of health is a situation that results in a life-threatening illness or injury or a permanent impairment of a body structure or a body function, requires in-patient hospitalization or prolongation of existing hospitalization, or results in medical or surgical intervention to prevent permanent impairment to a body structure or a body function.
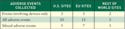
Recommendation. Responsible and rational adverse-event reporting is a continuing problem for all device sponsors. Most sponsors, regulators, investigators, and IRBs agree that ISO is too restrictive and CFR Part 812 is too confusing. An informal survey of device manufacturers in October 2006 indicated that most sponsors collect all adverse events regardless of whether the event is device related.
|
Table I. (click to enlarge) Responses of 26 medical device manufacturers when asked about their |
The following survey question, “Of the medical device or device-combination clinical trials you conducted in 2006, did you collect only device-related adverse events, all adverse events, or a mix of adverse events according to a plan your company developed?” was e-mailed to 100 companies outside of the United States and 200 companies within the United States. Table I is based on responses from 26 manufacturers.
It may be best to begin with the clause in the ICH-GCPs that allows reporting exemptions for those adverse events listed in the protocol (5.18.4). Then switch to the requirements of ISO 14155 and take advantage of its definition of a serious event as one that requires hospitalization.
Finally, procedures should follow the ISO requirements and take the following steps:
Review all adverse events that occur by training the monitor to review against the source document and ensure that they are properly categorized based on their seriousness and the degree to which they are related to the device (8.2.i).
Report all serious adverse device effects and all other serious adverse events to authorities, ethics committees, and monitoring boards as they occur (8.2.i).
Report all serious adverse device effects and other serious adverse events to other principal investigators as they occur (8.2.j).
Item. The ICH-GCPs provide for central monitoring when it is conducted in conjunction with procedures such as investigator training and meetings (5.18.3). Statistically controlled sampling for selecting the data must be verified (5.18.3). Neither element is discussed in the ISO standard.
Recommendation. Central monitoring can be used to verify completeness, legibility, logic, traceability, error-correction procedures, and presence of the investigator's signature. It covers nearly every element of case report form monitoring other than source verification. It can be an efficient tool for on-site monitoring visits. Sampling (i.e., source-verifying a subset of case report forms) is a common method for reducing on-site monitoring time and costs. Both methods should have a place in a company's corporate procedures.
Item. The ICH document says monitors should follow the sponsor's established written SOPs as well as those procedures that are specified by the sponsor for monitoring a specific trial (5.18.5). SOPs are not required by ISO's document.
Recommendation. It is worth noting that ICH assumes that firms have SOPs for monitoring clinical trials and that those SOPs can be customized for specific trials. SOPs are essential for the management of any clinical research program.
Item. The ICH-GCPs state, “The review and follow-up of the monitoring report by the sponsor should be documented by the sponsor…” (5.18.6). ISO 14155 is not as detailed and does not require that the sponsor review the monitor's written report or document that review.
Recommendation. A simple countersignature on the report will do, but the quality system should require it.
Item. The ICH-GCPs devote an entire section to defining the purpose of the audits, frequency of audits, having SOPs for auditing, how to conduct audits, and audit certificates (5.19.1–5.19.3). It also clarifies that regulatory authorities should not request audit reports. ISO 14155 has one sentence on auditing. It says, “The clinical investigator(s) shall allow auditing of their clinical investigation procedures” (Part 1-6.12).
Recommendation. Monitors work alone in the field. Therefore, auditing is a useful way to check their work. The frequency of audits should be commensurate with the product risk. However, it is appropriate for new monitors to receive an annual audit for each investigative site.
Section 6. This section covers trial protocols and protocol amendments. The contents of a protocol as described by ICH are basically the same as ISO, but there are some notable differences. ICH, for example, allows for a description of the stopping rules or discontinuation criteria for individual subjects, parts of the trial, and for the entire trial (6.4.6). The issue isn't discussed in ISO, but the value is apparent. One useful rule of thumb is that you can do anything you want in a clinical trial, as long as you say so in the protocol.
Item. ICH provides for data to be recorded directly on the case report forms, that is, without prior written or electronic records of data. These data are considered to be source data and are identified in the protocol (6.4.9). ISO doesn't mention recording directly on the case report form. In practice, certain forms are commonly completed while interviewing the participant. These types of interviews are considered both source documents and case report forms.
Recommendation. The protocol should specify criteria for discharging subjects from a trial early for, say, noncompliance to the protocol for failure to keep follow-up visits (6.5.3). Involuntary discharge of a subject from a trial is not discussed in ISO, but it is an essential management tool that should be incorporated into every protocol and clinical quality system.
Section 7. This section of the ICH-GCPs covers the investigator's brochure. According to the document, the purpose of a brochure is to provide investigators with the information to facilitate their compliance with the protocol (7.1). In cases for which preparation of a formal investigator's brochure is impractical, the sponsor or investigator should provide, as a substitute, an expanded background information section in the trial protocol. The section must contain the minimum current information described in this guidance (7.1).
Item. The contents of an ICH investigator's brochure are by nature pharmaceutically oriented. They include requirements such as highlighting the significant physical, chemical, pharmaceutical, pharmacological, toxicological, pharmacokinetic, metabolic, and clinical information available (7.2).
ISO asks for a more device-oriented content: a literature summary, list of materials and components, intended clinical performance, summary of relevant preclinical data, summary of previous clinical experience, list of international standards complied with, and results of the risk analysis (Part 1-7.2).
Recommendation. The ISO model is more closely suited to the needs of a device trial, and sponsors should use ISO to create the investigator's brochure.
Section 8. Section 8 of ICH-GCP is a comprehensive list of the documents that should be kept during the conduct of a clinical trial and a designation of who should keep them. The ISO standard does not have such a list and would benefit greatly from one. Firms should incorporate such a list in their company's clinical research quality system and document it in the SOPs.
Strategy for Success
By conducting the first-in-human and pivotal clinical trials in Europe or in developing nations, companies may have an easier path to get clinical trials started. In general, firms should choose countries with investigators trained in Western medicine. Selected countries should have ample patients for participation and an interest in implementing trials that will generate data sufficient for later submission to FDA.
Once the requisite trial is complete and you are ready to present your data to FDA, tell the agency that you have conducted ethical clinical trials in other countries. Further, tell FDA that you propose to do a confirmatory study in the United States.
When writing the clinical quality system SOP, it is best to methodically use the ICH-GCPs and bring in elements of ISO 14155 when appropriate. It is also important to incorporate checkpoints for host country regulations. Become familiar with the International Ethical Guidelines for Biomedical Research Involving Human Subjects.3 Be absolutely ethical in the conduct of the trials.
Through the process, OEMs gain an understanding of the expectations for conducting clinical trials, which increases the chance for market success. Use the guidelines and standards as intended, but don't be afraid to tailor these to your specific needs.
Nancy J. Stark is founder and president of Clinical Device Group Inc. (Chicago). She can be reached at [email protected].
References
1. ISO 14155:2003, “Clinical Investigation of Medical Devices for Human Subjects—Parts 1 and 2,” (Geneva, International Organization for Standardization, 2003).
2. ICH-GCP:1996, “Harmonized Tripartite Guideline, Guideline for Good Clinical Practice—E6,” (Geneva, International Conference on Harmonization 1996).
3. International Ethical Guidelines for Biomedical Research Involving Human Subjects, (Geneva, Council for International Organizations of Medical Sciences (CIOMS), 2002).
Copyright ©2007 Medical Device & Diagnostic Industry
About the Author(s)
You May Also Like


.png?width=300&auto=webp&quality=80&disable=upscale)
