Sensor Advances Spur New Diagnostic, Therapeutic Tools
Medical Device & Diagnostic Industry MagazineMDDI Article IndexOriginally Published May 2000SENSORSThe market for sensing technology continues to grow at a rapid pace, stimulated by new materials, novel design and fabrication methods, and innovative thinking.
May 1, 2000
Medical Device & Diagnostic Industry Magazine
MDDI Article Index
Originally Published May 2000
SENSORS
The market for sensing technology continues to grow at a rapid pace, stimulated by new materials, novel design and fabrication methods, and innovative thinking.
The ability to measure physiologic parameters is a key element of effective medical diagnosis and treatment. Accurate determinations of biologic variables such as pulse, respiration, blood oxygenation, and glucose levels are used by physicians to correctly identify most illnesses and conditions. Such measured values are commonly used in the course of treatment—often to monitor a patient's condition or to guide a practitioner's hands. Following a procedure, physiologic assessments are needed to determine how well the treatment has worked.
Sensors have traditionally played an important role is measuring and monitoring a broad range of physiologic parameters. All sensors perform the same basic function—the conversion of one type of measurable quantity, such as temperature, into a different but equally quantifiable value, usually an electrical signal. Although the basic function remains the same, the technologies used to perform that function vary widely.
 Sandia's "smart scalpel" provides instant feedback to surgeons, making them aware when all cancer cells have been removed from a tumor site. Photo courtesy of Randy Montoya and Sandia National Laboratory.
Sandia's "smart scalpel" provides instant feedback to surgeons, making them aware when all cancer cells have been removed from a tumor site. Photo courtesy of Randy Montoya and Sandia National Laboratory.
The technology behind sensor development and use has evolved significantly over the years. Sensors capable of measuring and recording bioelectric activity were explored during the early 1800s. Devices capable of measuring bioelectric events included the first electroencephalograph in 1875, and early electrocardiographs were developed soon after the turn of the century. Sensitivity and complexity increased as advances were made in electronics technology, including innovative circuit designs, the invention of vacuum tubes and transistors, and more-efficient power sources.
Sensors today are evolving more rapidly than ever—the result of microcircuits and nanotechnology, improved materials, and new design capabilities. "I believe that the advancement of microfabrication and nanotechnology in recent years will have a significant impact on biosensors," says Chung-Chiun Liu, PhD, professor of chemical engineering at the Case Western Reserve University electronics design center (CWRU; Cleveland). "Microfabrication technology can be used to produce geometrically well-defined, highly reproducible structures and surface areas. Consequently, this may simplify or minimize the need for individual calibration."
Current growth in sensing technology is expected to have a dramatic impact on many medical practices and on healthcare delivery in general. Innovations in sensor design are changing many aspects of medical care—guiding surgical procedures, enhancing diagnostic functions, and ensuring treatment efficacy.
SENSOR TYPES
Although a wide range of sensors can be used for biomedical applications, they all can be categorized generally as being either physical or chemical in nature. Physical sensors are used to measure a range of physical responses in patients, such as temperature, blood pressure, and muscle activity. In addition to the most common types of physical sensors—optical and electrical—the category includes geometric, mechanical, thermal, and hydraulic types. Sensors that detect electrical activity include electrodes that are common in both diagnostic and therapeutic usage. Optical sensors are being used in a number of applications in which light is used to collect physical data. They are a key element of certain new technologies, including lab-on-a-chip devices.
Chemical sensors are designed to detect or measure the presence of specific chemical compounds. They are often used to monitor the presence of particular chemicals in the body for diagnostic or therapeutic applications. This category includes gas and electrochemical devices. Photometric sensors, which are optical sensors used to measure chemical presence, are also included in this category. Although bioanalytical sensors are generally considered to be chemical sensors, they have been considered a separate category by some sectors of the industry.
Sensors can also be classified according to the interface that exists between the sensor and the patient. They can be noncontacting or noninvasive, which clearly involves the least interaction between patient and device; skin-surface, which entails minimal patient-sensor contact; indwelling or minimally invasive; and implantable, which requires an invasive procedure to place the sensor. The type of patient-sensor interface to be established plays a significant part in sensor design and material selection. Noncontacting and skin-surface sensors offer the fewest limitations and the lowest potential risk. Where indwelling and implantable sensors are required, however, issues such as rejection reactions and how such reactions affect sensor function become critical. In addition, normal biologic function can affect sensor activity, creating conditions that can degrade sensor performance. Sensor design and selection of the materials used in the sensor package must reflect such considerations.
The sensor package itself is a critical design challenge. The package must maintain an adequate barrier between the sensor components and the essentially hostile environment of the human body; however, it must also allow the sensing components to maintain contact with the relevant biologic systems without loss of calibration. Much of the current research involving sensor technology is focused on developing sensor packaging that allows full function and durability—without increasing sensor size.
SENSORS IN THE SURGICAL SUITE
Sensors have long been used in surgical settings for patient monitoring during procedures. Sensors to measure respiratory parameters, blood gases, pulse, and blood pressure are needed to continually assess the patient's condition throughout a surgical procedure. Recently, sensor technology has been adapted to guidance applications, extending the capabilities of surgeons. Applications in microsurgery and robot-assisted procedures are proving to be especially promising.
Sensors Guide Tumor Removal. Researchers at the U.S. Department of Energy's Sandia National Laboratory (Albuquerque) have developed a sensor-based mechanism to help surgeons remove cancer tissue. Called a "smart scalpel," the patented device essentially is capable of telling the surgeon when to stop cutting to avoid removing healthy tissue. The system uses microchip-connected sensors to provide "instant feedback to the surgeon" performing the laser procedure, according to the researchers.
Conventional lasing methods immerse the blood cells in laser light—like a spotlight. The dime-sized Sandia device incorporates the cells into the lasing process itself. The beam of a vertical microlaser scans individual cells pushed by a micropump through tiny channels in the device. Cancer cells contain higher concentrations of protein than normal cells, causing greater density. The increased density results in refraction, altering the laser light passing through the cancer cells. The device registers this change as a difference in output frequency and transmits the data to a laptop computer near the instrument. The data are translated by an algorithm into a continuous graph that allows surgeons to determine when all cancerous cells have been cleared.
Relying on microsensing capabilities, the device has been found to yield results more quickly than flow-cell cytometry—the conventional method for detecting the presence of cancer cells in samples obtained by incision. "We can quickly identify a cell population that has abnormal protein content, as do tumor cells, by passing only a few hundred cells—a billionth of a liter—through our device," says Paul Gourley, who leads the Sandia research team. "People didn't believe we could pump cells through a microlaser, make the cells part of the lasing process, and produce meaningful results. As it's turned out, we can do all these things." Gourley describes the technology as being "like an instantaneous lab report on a biopsy."
Steve Skirboll, MD, of the University of New Mexico School of Medicine (Albuquerque), is helping determine characteristics of the system. "The device has great potential benefit, particularly if we continue to develop the nanotechnology at its base," Skirboll explains. "We're still looking at the basic science to nail down the major determining factor, but the results are encouraging. We can show differences between tumor and nontumor cells for the cancer we're examining."
The device is still in early stages of development, and it has been used only on cultured cells to date. Sandia researchers suggest, however, that further development of the microsensing element could extend the device's capabilities. The researchers suggest that it is also capable of detecting other blood-protein abnormalities, including sickle-cell anemia.
Enhanced Microsurgical Techniques. A robotic-assisted microsurgery (RAMS) system was recently described during the annual meeting of the American Association of Neurological Surgeons (AANS) in San Francisco. The prototype was developed by NASA, the Jet Propulsion Laboratory, and MicroDexterity Systems (Memphis). The system enables surgeons to direct the motions of the robotic instrument by using a master input handle that resembles a surgical tool. A computer system processes the surgeon's movements in real time and transfers them to the robot. Sensors incorporated in the instrument generate signals that are modified by the computer and used to monitor the instrument's position and movements. The system is designed to reduce the surgeon's movements at the tissue level. It can also prevent incorrect moves and reduce tremor caused by anxiety, fatigue, or age, according to the researchers.
"The role of the robotic-assisted system is to enhance and standardize a procedure," says New York neurosurgeon Peter LeRoux, MD, who described his experience with the system during the AANS meeting. Surgical results and error rate using the system have been found to be similar to those obtained with conventional surgical techniques.The RAMS system is intended for use in a range of microsurgical procedures, including repair of cerebral aneurysms, anastomosis of blood vessels or nerves, brain tumor resection, and acoustic neuroma removal.
Thermoregulation during Surgery. Patients undergoing general anesthesia during surgery are vulnerable to hypothermia. When the body temperature drops below normal, various medical complications can result, including slow recovery, increased morbidity, and death. MTRE Advanced Technologies Ltd. (Or Akiva, Israel) has developed a system for controlling body temperature of patients during surgery. The Allon thermoregulation device consists of three components: a disposable garment of synthetic fabric that wraps around the patient's body, temperature sensors, and a microprocessor-controlled heating/cooling unit. The sensors provide a feedback loop between the patient and the heating/cooling unit.
Tubing between the garment and controller unit allows water to flow between the components. The sensors enable the device to pick up slight shifts in patient temperature during procedures. The controller unit then circulates warmer or cooler water as needed to maintain a stable temperature. "All the physician has to do is set the desired temperature, and the Allon system maintains that level," says Igal Kushnir, MD, CEO of MTRE. The system, which was recently approved for marketing in the United States, has been tested during clinical trials involving pediatric and open-heart surgery at hospitals in Israel. It has also been studied during resection of abdominal tumors and liver transplants performed at Vanderbilt University Medical Center (Nashville, TN).
THE SHAPES OF THINGS TO COME
The key to breakthrough developments is often as simple as looking at a problem or situation from a new perspective. Researchers at Ball Semiconductor Inc. (Allen, TX) have applied this technique in developing a novel circuit concept that is shaping the future of sensing technology. The researchers, led by Suzanne Ahn, MD, director of the Ball medical division, have designed a circuit with a spherical geometry that is expected to dramatically influence medical sensor technology. The firm's 1.0-mm spheres provide more than three times the usable surface area of conventional flat chips of equal size. Ball expects to eventually reduce the sensor's size to 20 µm, or about 0.0007 of an inch.
The spherical geometry allows a circuit placed on the chip to be wound around the surface to create a property of inductance. "The added dimension of height provides for much greater inductance values than that which is achievable on flat chip surfaces," according to Ball. The firm explains that windings can be used as an antenna to provide wireless communication between sensors implanted in the body and peripheral devices. The results, the company suggests, would be sensors with true 3-D acquisition capabilities. Sensors placed on the sphere's surface would be multidirectional and capable of generating data that are more comprehensive than conventional sensors.
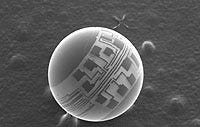 Ball Semiconductors' spherical chip could produce 3-D sensing capabilities. Applications include sensor-tipped catheters, implant markers, and swallowable vital signs sensors. Photo courtesy of Ball Semiconductors Inc.
Ball Semiconductors' spherical chip could produce 3-D sensing capabilities. Applications include sensor-tipped catheters, implant markers, and swallowable vital signs sensors. Photo courtesy of Ball Semiconductors Inc.
Says Ahn, "Basically, what we want to do is get rid of the wires, the cables, and all the tubes that encumber a patient." She explains that the inexpensive sensor could be swallowed by a patient and it would monitor vital signs with 3-D sensing capability. She also suggests that the technology could be used in operating rooms to track surgical instruments and sponges. "When you have major surgery, the doctors have to do a sponge count before opening and before closing the patient to make sure nothing gets left behind. It's done by hand and, if you have a miscount, you have to bring an x-ray in and read the film and locate where you may have left something." The electronically tagged instruments could be located with a simple scanner, she says. Other potential applications of the spherical chips are sensor-tipped catheters or guidewires, wireless electrodes, implantable neurostimulation devices, and a proprietary chromatography technique.
In addition to reexamining the optimal shape of sensing devices, dramatic reduction in sensor size is making new applications possible. Integrated Sensing Systems Inc. (Ann Arbor, MI) is developing a pressure sensor that is only 0.25 mm wide, small enough to fit inside the eye of a needle. Because the device can be placed inside most catheters, the technology potentially could offer multiple possibilities, the firm states. A single sensor could be used to measure the internal pressure of organs or wounds. With a pair of the devices, a pressure drop across an arterial obstruction could be measured. A sensor array could be used to characterize flow across long arterial or intestinal sections. When manufactured, the microsensor is expected to provide a pressure range of 0–1200 torr, and resolution of <0.3 torr.
REPLACEMENT OF ORGAN FUNCTION
Combined with novel technology, sensors are providing the basis for devices that can replace the function of certain organs. For example, diabetes patients have been disappointed several times in recent years by premature claims that development of an artificial pancreas was near. New projects, however, are expected to yield substantial advances in diabetes care in the medium to long term.
Implantable Glucose Monitor. A microchip being developed by Sensors for Medicine and Science Inc. (SMSI; Germantown, MD) incorporates an optical sensor capable of detecting a wide range of analytes, including oxygen, carbon dioxide, pH, glucose, lactate, and anesthetic gases. The firm's oxygen sensor prototypes use a tiny light-emitting diode (LED) as the light source and an ordinary photodiode to measure the light output. Both low-cost components are widely available. A key element of the SMSI design is the placement of the excitation source in the sensor element. The LED is embedded in a matrix containing the fluorescent indicator molecules to overcome a number of technical challenges. "If you understand how light behaves in the presence of certain compounds, you can use light to detect the presence or absence of those compounds," says Arthur Colvin, who designed the sensor platform. "The hard part is using what you know to build a sensor that's stable, very sensitive, and inexpensive."
The small size and low cost of the SMSI sensor components are essential to new applications, including implantable microsensors, according to the company. Conventional glucose-monitoring systems require skin pricks and blood sampling. SMSI is now working on a sensor small enough to be injected into the fatty layer below the skin to measure blood sugar levels in diabetic patients. Sugar reduces the light reemitted by the fluorescent chemical. Basically, the higher the glucose level, the less light is detected. The implanted SMSI sensor would thus measure the glucose level by detecting the reduced light level. The result would be transmitted to an external unit via radio-frequency communication. The low-power unit, resting just beneath the surface of the skin, would be powered externally by induction.
The company indicates that the optimal fluorescent chemical remains in development; however, the chip design has been completed. The prototype device uses a 22-µW LED—a fraction of the power needed for the power-on indicators of most personal computers. Because the fluorescence detection process consumes no chemicals or proteins, the device is self-sustaining, according to the firm.
"Diabetes is a disease that typically attacks people when they are very young or as they begin to grow old," SMSI president and COO Marc Schneebaum notes. "Those are the times in people's lives when they may be most vulnerable. We think that's a very compelling reason for the work we're doing." Schneebaum adds that "an implantable sensor that could be powered up and queried on demand would go a long way toward helping diabetics manage the disease."
Artificial Pancreas. The Disetronic Group (Burgdorf, Switzerland), which produces insulin and injection pens, is conducting research to develop an insulin delivery system with integrated blood sugar monitoring. The goal of the firm's ADICOL (advanced insulin infusion with a control loop) project is to develop a prototype artificial pancreas that would automate daily insulin administration while maintaining dosage accuracy.
In addition to an insulin pump, the ADICOL system uses a glucose sensor implanted under the skin to continuously measure and display blood sugar concentration. An alarm is sounded if the measurement exceeds or falls short of threshold concentrations. Software enables the sensor to control the insulin pump, ensuring a precise insulin dosage.
Disetronic notes that it has brought together a promising consortium to advance its ADICOL project. The project currently includes research in clinical centers at the University of Graz (Austria) and the University of Perugia (Italy); sensor technology development at the Fraunhofer Institute for Biomedical Engineering and SensLab GmbH, both in Germany; and the City University of London and Judex A/S (Aalborg, Denmark), which are providing expertise in control algorithms and simulation models.
SENSORS FOR DIAGNOSIS AND MONITORING
A number of new sensing technologies are proving valuable for bioanalysis—improving the detection and monitoring of diseases. New systems that are smaller and easier to use are offering a broader range of diagnostic capabilities. They are also providing more-effective methods for monitoring specific disease conditions.
Sicel Technologies (Raleigh, NC) is working on a sensor-based monitoring technology that could be used to assess the effectiveness of cancer treatments. A prototype in current development uses a sensor that would be implanted within a tumor. Combined with a miniature transmitter and receiver, the sensor would generate data about the tumor's response to chemotherapy or radiation treatment. By determining whether or not a tumor is responding to treatment, the system reduces the need for oncologists to rely on guesswork to plan ongoing therapy.
Currently, oncologists must determine a course of treatment based on data provided by biopsy or diagnostic images. How well a given tumor will respond to treatment is largely guesswork. Tissue samples and images provide only brief glimpses of tumor condition. "That's one point in time," says Charles Scarantino, MD, PhD, cofounder of Sicel. "Once you begin treating the patient, everything changes. And it changes in a way you can take advantage of, if you know what is happening." For example, chemotherapy performed when a tumor is in a growth phase is generally more effective than during other phases. And the performance of drugs can change in response to variations in the body's pH.
 The microdialyzer biosensor developed by Sycopel combines in vivo microdialysis and voltametry in a single unit and facilitates analyte monitoring. Photo courtesy of Sycopel International.
The microdialyzer biosensor developed by Sycopel combines in vivo microdialysis and voltametry in a single unit and facilitates analyte monitoring. Photo courtesy of Sycopel International.
The first sensors developed by Sicel were 6-sq-in. circuit boards. The current version is 1 cm long and 2 mm wide, and can fit within a typical biopsy needle. Initially, the sensors will be used to monitor radiation levels and temperature within tumors. Radioactive tags attached to cancer drugs would allow the sensor to measure uptake of the drug by the tumor. Eventually sensors will be used to assess other aspects of chemotherapy, according to the company. Although the first sensors will require patients to come to a clinic and don a transmitter/receiver-equipped vest for testing, the system may eventually use a wireless system that would allow continual monitoring of the patient at home via laptop or desktop computer.
Other sensor systems are being developed to increase flexibility of certain aspects of testing. A microdialysis biosensor being developed by Sycopel International (Jarrow, UK) integrates in vivo microdialysis and voltametry functions in one unit. Conventional techniques require samples to be collected at intervals with a microdialysis probe—increasing test complexity. The microdialysis system can be used for real-time measurement of analytes in vivo, which simplifies the analyte testing process.
The microdialysis biosensor includes a platinum wire set inside a hollow semipermeable membrane. Two vitreous silica tubes are used for solution exchange within the probe. This provides the device's ability to control the microenvironment of the working electrode. Enzymes or biologically active molecules are replaced within minutes if they become inactive, or if the specificity of the biosensor is to be changed by using a different enzyme. Two additional electrodes—a silver or platinum counter and a silver/silver chloride reference—comprise an electrochemical cell. This cell is located away from the main sensing area, in a glass or steel compartment. The ends and the joints are sealed with epoxy. Stainless-steel recording electrodes attached in parallel to the membrane allow field potential recording during concomitant electrophysiological studies. The electrodes can be used to position the biosensor and for subsequent activity recording.
Sycopel states that the microdialysis biosensor offers a number of advantages over conventional analytical methods. Specifically, the "internal plumbing system" of a single microdialysis biosensor can perform both control and measurement analyses in one tissue area without being moved. Additionally, different enzymes can be added to change the biosensor specificity for comparison of different analytes. For example, glucose and lactate concentrations can be compared using the same electrode in a brief time period. The biosensor has been shown to be capable of measuring small physiological changes involved with learning and memory in vivo, and during activity in the freely moving rat. Studies have also assessed use of the system for drug evaluation and in vitro bedside monitoring of human glycerol levels. The firm indicates that current research with the device includes long-term potentiation, epilepsy, drug evaluation, and behavioral studies.
CONCLUSION
The future of sensor technology is being influenced significantly by current developments in miniaturization and microarrays. Development of "smart devices" and intuitive systems for patient treatment also rely on the progress being made in sensor technologies.
Researchers and engineers are being challenged to consider new perspectives on sensor design and fabrication. Says CWRU's Liu, "The use of a sensor array for multiple detection on a small sample will increase." He explains that "microfabrication technology will continue to be used for sensor development. However, one must recognize that silicon is not really biocompatible. Consequently, microfabrication processes of nonsilicon, nontraditional materials will have to be developed or modified based on silicon-based processes."
Liu explains that microfabrication also allows the production of a sensor array that can perform multiple measurements using a microsized sample. "I want to emphasize the importance of using an array for multiple detection, which is very desirable for biomedical applications. In terms of sample size for blood sampling, 80 µl—approximately 2 drops of blood—for multiple sensing of as many as eight parameters is a design goal for many sensor companies."
He further suggests that soon-to-be-developed sensor technologies will have dramatic benefits for diabetic patients. He states that increased availability of low-cost glucose sensors for diabetic management in the past decade has been an important development. "This is because the size of the diabetic patient population is extremely large, and the benefits can be appreciated readily." Innovative systems for diabetes control may also become available in the near future, Liu says. "Because of advances in sensor technology combining with progress in computer hardware and software, closed-loop control in a biological system seems feasible. Therefore, increasing activities are taking place in the development of an insulin-delivery system." He adds that "this will not be feasible unless a reliable small-sized glucose sensor is available."
Liu also suggests that there will be an increasing need for new sensor-based devices for home-care and point-of-care applications. He explains that these products will require reliable, robust, and simple sensor arrays.
Commenting on challenges to sensor development, Liu suggests that "one of the important but often overlooked challenges in biosensor development will be packaging. On one hand, we need to expose the sensors to the bioenvironment, which is less than friendly. On the other hand, we need to protect the integrity of the sensor, and we need to cover the device as much as possible. Consequently, research on biomaterials will be important for developing biocompatible coatings."
Gregg Nighswonger is executive editor of MD&DI.
Return to the MDDI May table of contents | Return to the MDDI home page
Copyright ©2000 Medical Device & Diagnostic Industry
About the Author(s)
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
