The Challenges of Getting Materials Innovations into Human Bodies
May 13, 2015
A University of Texas at Dallas researcher and his team have developed innovative flexible, shape-shifting electronics. But that is just the beginning.
|
Walter E. Voit |
Chris Newmarker
A University of Texas at Dallas researcher has figured out how to "program" shape-shifting thiolene/acrylates embedded with electronics to wrap around nerves as thin as 60 microns across. Imagine neurological conditions treated with minimally invasive electrodes wrapped around nerves at strategic places in the body.
And yet as impressive as the achievement sounds, Walter E. Voit has some significant technological challenges to solve in coming years if his tiny, shape-shifting electronics are going to be used in human beings. His story provides a great example why it can take so long for medtech innovations in the laboratory to make it into the human body--if they ever do.
Voit and his team have already accomplished a great deal with their research, which is backed by the U.S. Defense Advanced Research Projects Agency (DARPA) and GlaxoSmithKline, among others. (See Voit discuss his research at MD&M East, June 9-11 in New York City.)
Not only can the thiolene/acrylates be engineered to change shape in a specific way when exposed to warm temperatures inside the body, but they have great adhesion with metals such as gold--which makes them a highly useful flexible electronics material
"I think what we've been able to do over the past year is really push the envelope on what we can do with these implantable node electronics," Voit says. "We've been able to build a series of implantable neural devices that can wiretap the body's nervous to record, block and stimulate individual action potentials across the central and peripheral nervous system."
Great challenges, though, lie ahead, according to Voit. "It's less trivial to demonstrate that these devices work acutely in animals and physiological conditions. But the real challenges are to understand in the aggressive environments of the body how these devices will survive and continue to operate over longer periods of time. That poses very interesting, fundamental materials questions in terms of interface physics, in terms of packaging and encapsulation."
|
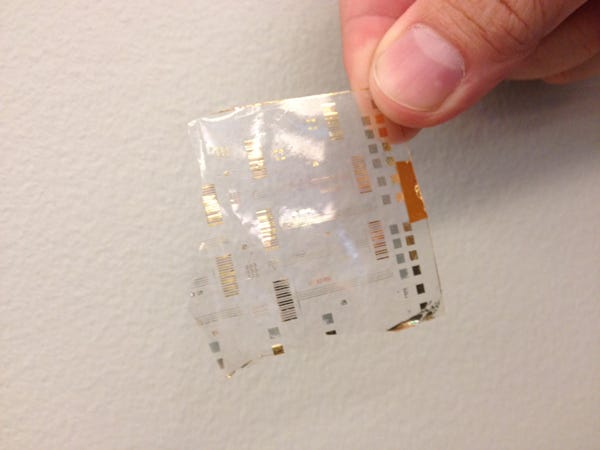
Walter E. Voit, assistant professor of the University of Texas at Dallas, holds semiconductor electronics embedded inside a thiol-based polymer film. The matrix-addressed transistor arrays used to stimulate nerves in a rats brain. |
Here are two of the major challenges Voit and his team need to overcome:
Making Sure It Stacks Up
The shape-shifting electronics are made by using additive and subtractive steps to create electronic components on gate stacks with as much as 15 layers, each anywhere from 3 nm to 10s or 100s of microns thick, Voit says.
Voit and his colleagues have been experimenting with a host of conductive materials in between the layers of thiolene/acrylates, including gold, titanium nitride, platinum, iridium, iridium oxide, carbon nanotube, graphene, semiconductors, and organic semiconductors.
None of this is encapsulated in the tradition "metal cans" one sees with electronic medical devices.
"You have to be aware of the tethering forces. You don't want to damage the nerves. You want to be able to measure them and interact with them closer to their natural environment," Voit says.
The shape-shifting electrodes have worked over the short-term inside rats. But what about the long-term inside human bodies?
"There's a lot of fluid. There's a lot of motion where there can be delamination, conductor cracking. ... We have to engineer these stacks so that when devices are inside the body and there are subjected to bending and contortion and stretching, that these stacks don't all pop apart from each other," Voit says.
The shape-memory polymers solve one piece of the puzzle. "But there are a lot of other pieces that are necessary when we're engineering these semiconductor-containing gate stacks to build highly functional devices."
Where Is It Useful?
The goal is to miniaturize a lot of the existing technology that's being used to interact with the nervous system, Voit says. "We're using new materials, new semiconductor processing approaches to be able to build our electrodes closer to the scale of biology, which will allow us to be more selective, more sensitive, more targeted to understand and control the nervous system."
But where should the electrodes be applied to best treat conditions. "We are actively working with some of the leading clinicians across the country to do that," Voit says.
Research collaborators include Jason B. Carmel, MD, PhD, who is exploring spinal cord stimulation and muscle plasticity at Cornell; Pankaj Jay Pasricha, MD, a leading gastroenterologist based at Johns Hopkins Medicine; Robert J. Butera, PhD, a bioengineer at Georgia Tech; and Mario Romero-Ortega, PhD, a bioengineer at UT Dallas.
"Those are the people who are working to undersand the fundamental neuroscience questions," Voit says. "The material scientists who can be useful in this are the ones who have these really tight collaborations with neuroscientists and clinicians where you can understand not only materials, interfaces and electronics, but how they behave inside animals in the body in these specific biological tests."
The wireless technology Voit and his team are designing for the shape-shifting electronics is in the in vitro stage, so the research mostly involves running connector wires into rats, using the shape-shifting electrodes as the interface with the nerves.
They are seeking to figure out where the interfaces are the most useful.
"I think gone are the days when you can design this generic mousetrap and have it work for a lot of things," Voit says. "I think the complexity of the body is such that to interact at the scales we want, it's going to take a lot of back and forth with leaders who understand the anatomy and physiology well and can help come up with the right animal models, the right tests, the right stimulation paradigms to get that work."
See Voit discuss his research at MD&M East, June 9-11 in New York City. |
Chris Newmarker is senior editor of Qmed and MPMN. Follow him on Twitter at @newmarker.
Like what you're reading? Subscribe to our daily e-newsletter.
About the Author(s)
You May Also Like