How to Prepare for the Internet of Things in Healthcare
August 31, 2015
How should medical device developers plan for the integrating the Internet of Things (IoT) into their products? Look to the past, says Bill Betten, principal at Sysgineering Solutions based in the greater Minneapolis-St. Paul area. And then follow the money.
Brian Buntz
|
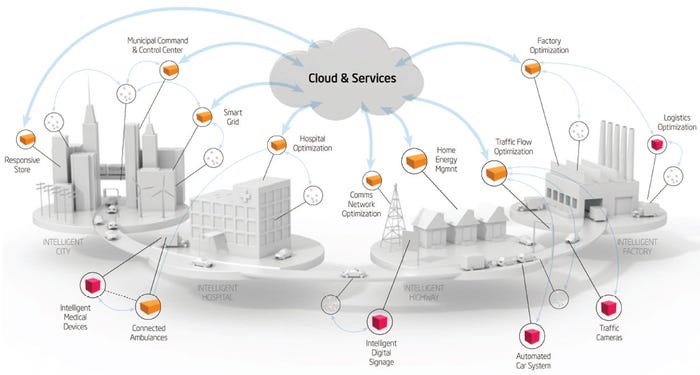
The IoT of things in healthcare could link ambulances, medical devices, and hospitals with integrated cloud-based services. Image courtesy of Intel. |
Proponents of the IoT say that it will revolutionize healthcare, making treatments smarter and better tailored to the needs of individual patients while curbing medical errors. In addition, the IoT has been predicted to advance how costly chronic conditions like heart diseases and diabetes are monitored.
Some predictions are more detailed. A report released last year by the Swiss research firm Soreon Research states that, by 2020, connected wearable devices alone could save an estimated 1.3 million lives. A report from MarketResearch.com estimates that, by 2020, the IoT market in healthcare will be worth $117 billion.
But how should medical device developers plan for this vision of the future when cybersecurity seems to be a growing risk in healthcare? And how should engineers plan for a future of widespread data sharing when much of the healthcare data is now still shared in a piecemeal fashion? And how can product developers separate IoT hype from reality?
While questions like those remain tough to answer, many new medical devices will have to be connected to be competitive, says Bill Betten, principal at Sysgineering Solutions who has worked for firms ranging from Nonin Medical to Logic PD to 3M. "One should definitely take advantage of the connectivity by building it in; it is hard to add it in after the fact," Betten says. And from a cost perspective, the bill of materials cost is much less of a concern in a med device than in a consumer device sector where you are fighting for every last inch of space, and every Joule of power.
"But I would encourage device companies to have a conversation around the strategy for incorporating that connectivity into the future product offering," he says.
1. Look Back to Look Forward
|
Bill Betten will share his thoughts on the IoT and healthcare at MD&M Philadelphia. |
It helps to have a historical perspective, Betten says. "I would argue that a lot of medical connectivity started in the late 80s and 90s. Looking back to this time period can give useful perspective in understanding what is happening in with IoT in healthcare," says Bill Betten, a medtech consultant with a development background in devices ranging from hearing aids to vital signs monitoring devices to medical imaging PACS. (Betten will speak on the subject at MD&M Philadelphia, which will be held this year from October 7-8.)
In the 1980s, there was a push to digitize radiology-based imaging, but there were technology- and standard-based hurdles that made it difficult to do so. By the 1990s, several manufacturers had developed methods for viewing radiology images electronically, but they were proprietary. It wasn't until 1997 that The New York Times declared that digital x-ray systems were beginning to replace film-based x-rays.
A big part of what enabled this to happen is the DICOM standard, which evolved from the ACR/NEMA 300 standard that was finalized in 1985 and was first given the name DICOM in 1993.
"Before DICOM, almost all radiology images were disconnected. You would shoot an image at a plate, develop the film, then you have an image that goes to an office to get read by a radiologist, and is later a filing cabinet," Betten recalls. "But DICOM enabled images to be shared worldwide, films to be duplicated, and machines from different manufacturers to communicate. Other devices such as blood pressure cuffs and pulse oximeters have similarly benefited from Continua's support of standards."
"So the first lesson of the Internet of Things is you need to be interoperable," Betten says.
2. Follow the Money
The second lesson concerning integrating the IoT into medical devices is to study its value proposition. "That will lead you to the question of what is your business model? Just because you can connect, why should you and what should you do with it?" Betten asks. "If you are going to connect your device, how are you going to monetize it? Are you going to make the most money from selling the device or selling a subscription?"
Betten also suggests studying the broader IoT healthcare landscape to determine how much money is being spent on using the technology for disparate applications. "Following the money will be important at determining the rate of adoption in healthcare," he says. "While you can see that a fair amount of money is being spent to incorporate the IoT in the smart home sector with things like connected thermostats, doors, and windows, it is not clear what the utility is there. In that niche, the technology is cheap enough and gadgety enough that the early adopters pick it up. But the medical world is a completely different environment."
While there is currently not a lot of data relevant to this subject, perhaps monitoring of the chronically ill is where the most money is being spent now. "According to Forbes (January 10, 2013), 5% of the sick population is responsible for 50% of the healthcare costs. I would suspect that the strongest case can be made for investing in the IoT to try to bring down those figures and make monitoring of chronic diseases like diabetes more efficient and effective," Betten says. "The finances around how the Internet of Things might benefit wellness are much less clear."
3. Ask Lots of Questions
As with any new technology, separating hype from reality can be a challenge. Even if the IoT makes good on its promise to help save the healthcare infrastructure hundreds of millions of dollars, it is not exactly clear how the IoT can do that. "Where do the savings come from? Hospitals need patients running through their system to make money. If hospital beds across the country were only half full, there would be a great cost savings. But you would have facilities that would close, and doctors that would be underemployed.
Thorny topics like this can make predicting how a healthcare technology will be adopted difficult. Consider electronic medical records. A decade ago the conservative think tank Rand published a study that found "effective EMR implementation and networking could eventually save more than $81 billion annually--by improving health care efficiency and safety--and that HIT-enabled prevention and management of chronic disease could eventually double those savings while increasing health and other social benefits." The report went on to assert that interoperable EMR savings could ultimately enable savings of $142-$371 billion, but adds the disclaimer that such savings are "unlikely to be realized without related changes to the health care system."
A decade later, EMRs have largely failed to substantially bring down to healthcare costs.
But the problem is likely not technological. A technology may like EMR or IoT may have immense potential, but yet fall short of its promise as a result of complex political, social, or economic reasons.
It's important to keep that reality in mind amidst talk of how healthcare is moving from therapeutics to encouragement of wellness. "There is no question that the numbers show that a healthier workforce is more productive. Healthy employees don't miss work," Betten says. "But how do you drive the behavior needed to make people healthy?"
But what mechanism is there now to pay for wellness?
There is clearly a need for technologies like the IoT, which could potentially help nations like the United States, Japan, and Germany help care for their ill as their population ages, but product developers should think long and hard on the strategy to do so.
There are also security concerns. As financial institutions become more adept at protecting their customer's money, hackers are looking to more towards identify theft, which more frequently means hacking medical-related data so they can glean social security numbers and so forth. This is not just a problem for health insurers. Last year, hackers acquired health data from Medtronic, St. Jude Medical, and Boston Scientific.
And then, of course, there are also technical concerns to weigh. And as the IoT becomes more common in the medical device realm, medtech engineers are being forced out of their comfort zone. "Medical device development personnel are good at understanding sensors, the device that drives it, because that has been the realm they have lived in," Betten says. "Now as we start to talk connections, you start to get into tradeoff scenarios: what is my power dissipation, what kind of data am I sending, how often do I have to turn on my transmitter, should I use Bluetooth Low Energy or WiFi? Do I want to take data to a hub or the cloud? Do I go to a smartphone or do I make a dumb hub? If I am up in the cloud, who is going to access it? And what kind of data is the most meaningful? And how do I ensure that this data is accessible in the long run--potentially decades from now?"
When coming up with a game plan for how to use the IoT in a product, Betten recommends thoroughly considering the following topics:
Sensors and Data
What data do you need to gather?
Does the equipment already have the required sensors built in?
Power
What is the amount of data needed?
How frequently will the data be collected?
Security
Protecting the data at collection, in transit and on the application.
Network Connection
What connection option best fits your application? Wi-Fi, Bluetooth, cellular, and other options?
Analytics
Data needs to be converted to useful information.
What is it exactly that your users want to know?
For the IoT to be meaningful, you need interoperability, security, and a reason for putting it together, Betten says. And a knack at coming up with good answers to tough questions.
Learn more about cutting-edge medical devices at MD&M Philadelphia, October 7-8, 2015. |
Brian Buntz is the editor-in-chief of MPMN and Qmed. Follow him on Twitter at @brian_buntz.
Like what you're reading? Subscribe to our daily e-newsletter.
About the Author(s)
You May Also Like