How a Jet Engine Sensor Became a Tiny Heart Failure Monitor
July 8, 2015
The sensing technology at the heart of the CardioMEMS HF system was inspired by a MEMS sensor designed to monitor the pressure within jet engines.
Brian Buntz
|
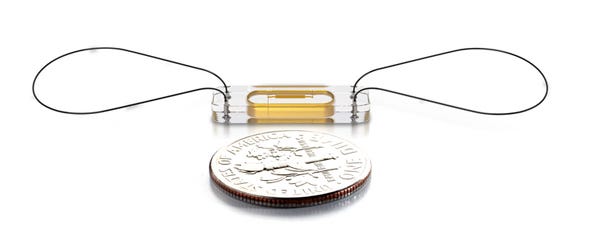
The current version of St. Jude Medical's CardioMEMS HF device is about the size of a paper clip. |
A decade ago, Jay Yadav, MD, former director of vascular intervention at the Cleveland Clinic, had the idea of taking pressure sensor technology designed for jet engines, and using it inside the pulmonary artery. Both were tubes, after all.
"They could ping the sensor with radio-frequency energy and measure the pressure inside of the tube," Philip B. Adamson, MD, medical director and vice president of medical affairs at St. Jude Medical, said of the technology, which was developed at Georgia Tech.
Yadav went on to found CardioMEMS to commercialize the idea, which was ultimately acquired by St. Jude Medical in 2014.
The sensor was given its first medical application in vascular medicine. "It was initially approved by FDA to be put into the exclusion sac of an aortic aneurysm that was fixed from an endograph," Adamson says. "Yadav said: 'I bet we could put this in the pulmonary artery and interrogate it.'"
In 2005, Yadav reached out to Adamson and Bill Abraham, now the associate dean for clinical research at the Ohio State University Wexner Medical Center, and asked the two to design a trial of hemodynamic monitoring of heart failure patients using MEMS technology.
When the two first heard about the technology, they were intrigued by the potential advantages of MEMS technology, which has a much smaller form factor than the can-type design traditionally used in cardiac rhythm management devices. (The current version of the device is roughly the size of a paper clip.) "We thought: 'gosh, it should survive the confines of a jet engine, it can survive the environment within the human body,' and sure enough it did."
The two men went on to help design the clinical trial, and eventually complete it.
"The Champion trial results were pretty profound: patients for whom there had been no therapeutic sequence or strategy or medicine to help them, this was the first time that a strategy helped them stay well and out of the hospital. There was about a 50% reduction in hospitalizations, and it was statistically sound. They represented about 25% of the population in the trial," Adamson says.
The CardioMEMS device obtained FDA approval in 2014.
For Adamson, the CardioMEMS device is a culmination of a changing philosophy that began to emerge in the mid-1990s in cardiology. About two decades ago, the notion of using hemodynamic monitoring to treat heart failure patients was just starting to take hold, he says. "At that time, electrophysiologists were becoming prominent in the management of heart failure," Adamson recounts. "We developed a hypothesis that the therapy we were delivering from the cardiac rhythm management devices we were implanting sensed a lot of information about the heart in order to deliver the therapy. We thought we might be able to harness some of that information to get a better handle on how patients with heart failure were doing," Adamson explains, who in 1995 had founded the Heart Failure Treatment Program at the University of Oklahoma and went on to found the Heart Failure and Pulmonary Hypertension Treatment Institute at Oklahoma Heart Hospital in 2005.
"One of the most important things in the heart failure disease management program is frequent assessment of the patient," Adamson says. "You hope that by doing that, you are going to catch things things that would lead to hospitalization and by catching them early, you proactively manage them and keep them from decompensating." But decades ago, frequent assessment meant seeing a patient at a weekly interval. "Because the vast majority of the patient's time is spent at home, we always felt there should be some way to monitor them there that would be better than having them report just their daily weight."
The late 1990s and early 2000s saw the launch of several clinical trials to test new methods of monitoring heart failure patients. In a number of trials, Medtronic tested combined cardiac resynchronization and implantable cardioversion defibrillation in their Chronicle device, which was an ICD that had the ability to monitor the pressure inside the heart as well as body temperature, patient activity and heart rate.
Adamson was the principal investigator of Medtronic's Reduce HF trial, which coupled the Chronicle device with a single chamber defibrillator. "Launched in 2006, that trial ended because that technology was kind of old and lead-based and pacemaker-like," he says. "All of the things that went with pacemakers went with that: lead dislodgement, pocket infections, and all of that stuff. Because the technology was less than optimal, the sponsor decided to abandon that project."
At roughly the same time Medtronic was abandoning their Reduce HF trial, Yadav reached out to Adamson to help design a clinical trial for it, which ultimately persuaded FDA reviewers of its safety and efficacy. "The risks of implantation are incredibly low, you don't have to replace the battery, you don't have to replace the device, and it lasts as long as the patient," Adamson says. "When you have the tremendous benefit that we found in the Champion trial, it really makes it pretty easy to accept as a technology to change the way we do things."
Refresh your medical device industry knowledge at MEDevice San Diego, September 1-2, 2015. |
Brian Buntz is the editor-in-chief of MPMN and Qmed. Follow him on Twitter at @brian_buntz.
Like what you're reading? Subscribe to our daily e-newsletter.
About the Author(s)
You May Also Like