Pivoting the Value for Flexible Hybrid Electronics
Technologies are accelerating applications that promise great strides in helping healthcare providers mitigate and minimize cross-contamination challenges during times of low-touch, no-touch interactions, social distancing—and beyond.

Monitoring vital patient information, such as blood pressure, respiration, temperature, and pulse, are routine and familiar duties at most healthcare facilities. During the current pandemic, however, these seemingly simple tasks are challenged by guidelines that limit close physical proximity.
While human contact is preferred to provide compassion and comfort as well as to meet certain compliance guidelines on validation of the collected data, this traditional approach is being reevaluated to minimize human interaction and risk exposure. As a result, medical device manufacturers now are looking at “digital health” solutions through an additional lens. Not only can wearable electronics help reduce ever-increasing healthcare costs, they can address self-monitoring demands when faced with a shortage of qualified healthcare professionals or an increase in cross-contamination concerns.
Transforming Healthcare with Wearable Tech Advancements
Flexible, wearable electronics, which leverage various industrial technologies and capabilities, promise a bright future for all types of frontline healthcare workers and facilities as well as the countless patients they serve. In particular, advancements in printed electronics, flexible hybrid electronics, electronics miniaturization, connectivity, artificial intelligence, cloud computing, wireless technologies, and power engineering play pivotal roles in the creation of vital monitoring platforms that no longer require large computers with a cornucopia of wires by the bedside or bulky handhelds carried around by healthcare workers and caregivers.
Flexible hybrid electronics-enabled sensors and devices can also be added in a large format on a single substrate that can be integrated into mattresses for monitoring situations like wetness and in some cases also provide therapy.
Instead, technology improvements will give patients the freedom and autonomy to self-monitor their vitals while ensuring data is attained and reported seamlessly without the inherent challenges of self-reporting. Wires and three-dimensional discrete buttons are eliminated by integrating electrical circuits and sensors directly onto product substrates with biocompatible adhesive plastics containing printed electronics. The technologies can also create sensor fusion by combining multiple sensors on the same substrate.
This integration makes it possible to measure a variety of vitals with the same device. It also makes the devices lighter weight, resulting in increased comfortability compared with traditional monitoring devices while also eliminating parts and/or simplifying the assembly process for manufacturers.
Connecting wearable devices to cloud computing platforms enable constant, automated reporting and monitoring via wireless connectivity. Powerful edge-computing, AI-based protocols create emerging opportunities to capture and deliver an entire spectrum of healthcare diagnostics, feedback, and even remedial instructions to patients for low-risk interventions. Initial trials already are underway globally to evaluate the benefits of these kinds of wearables in new low-touch or touch-free applications.
Smartphones and ‘Hugging Vests’ Help Patients Stay Connected
The ability to connect a new class of monitoring devices to smartphones or smart speakers results in immediate feedback and user guidance. Also on the drawing board: Wearable ways to collect and interpret speech and cough patterns to discern distinct markers of respiratory problems.
A wearable patch with acoustic and audio sensors or microphone then could deliver vital measurements—and continue to do so even when the wearer is at home. In some cases, functional inks can be used to print these sensors directly onto the substrates of the wearable.
To address the lack of human contact, touch, and presence that can provide comfort to patients, video conferencing with family members can be augmented by concepts such as “active hugging vests,” which provide gentle pressure with mechatronics, and touch-enabled wrist wearables, which can help fill the gap where risks of exposure are acute, especially in assisted living facilities.
Additionally, these flexible wearables can be made with a sensing biocompatible portion that wearers can dispose of after use while the accompanying encapsulated electronics module can be cleaned as per guidelines for continued reuse. In addition, low-cost versions of this device could be completely disposable—as long as the method complies with global and local regulations.
Reducing Cross-Contamination Risks with Wearables
The domain of wearable electronics may soon expand to include a wide variety of air quality monitors. While there still remain challenges with biochemistry and compatibility, such portable devices may integrate rapid diagnostic electronics with biosensors to allow pathogen detection. By collecting data from the air around the wearer, and then connecting and correlating that data to permissible medical records, wearers can be guided to areas with lower risks of exposure. Likewise, data collection is crucial to contact tracing, which is a highly effective public health strategy for fighting communicable diseases.
The use of diagnostic wearables and biosensor-equipped devices helps minimize risks of cross-contamination in settings where social distancing alone is ineffective or impossible. In addition, these highly effective devices can increase the efficiency of healthcare systems and their mitigation policies. In a “touch-free” healthcare environment, clinical staff are capable of monitoring patients who are in isolation or self-quarantine in remote and/or distributed locations due to their exposure to pathogens or other risks.
Spreading the Benefits of Technology Adoption
The applications for flexible hybrid electronics are not limited to wearable electronics. The same capabilities and capacities can actually help create solutions across a wide variety of healthcare applications.
For example, there is also an increasing need to understand the travel history of shared equipment and instruments across the facility to facilitate rapid contact tracing. The inclusion of wirelessly connected asset tags on industrial equipment, appliances, infrastructure, tools, and even transportation equipment like beds and trolleys can help automate tracing. Tracking inanimate assets perhaps will have a lower burden of privacy concerns.
Location tagging also can be used to validate authenticated delivery and tracking of devices and supplies. Therefore, in some healthcare applications, staff workloads can be reduced with the use of collaborative robots or cobots equipped with the ability to interact with miniature asset tags on supplies to pick and deliver replenishments to the patient bedside.
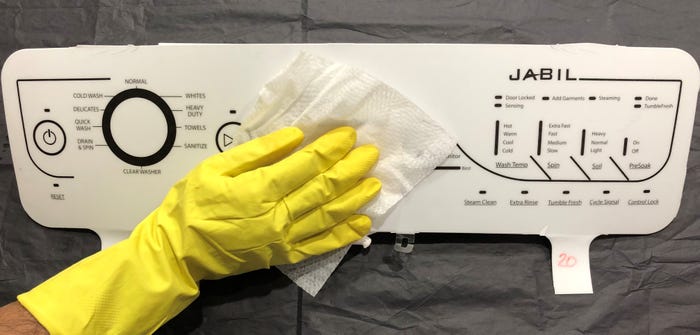
Equally important is the opportunity to add capacitive touch features leveraging flexible hybrid electronics directly onto plastic or glass surfaces to eliminate contamination-prone knobs, buttons, or expensive displays. Crevice-free, smooth human machine interfaces, which are easier to clean and maintain, are poised to drive the introduction and adoption of clinical and healthcare-related uses because of the opportunity to minimize cross-contamination. Furthermore, gesture recognition features, leveraging printed and flexible hybrid electronics, can be integrated in these surfaces to allow for “low-touch” interactions.
Similar printed capacitive trace features that enable human machine interfaces can be added to liquid bottles of disinfectants and sanitizers in order to monitor their use; when connected to monitoring devices, they can alert facility staff of low levels requiring replenishment.
Shifting Value Propositions
The biggest result of innovations in wearable, flexible, and disposable technology—beyond the lifesavings benefits realized from the growing roster of connected health applications—is the shift in value propositions. What began powered by the need for cost reductions and then expanded to include comfort, convenience and independence, has shifted further to incorporate the urgent need to minimize contact as well as prevent cross-contamination and unneeded exposure to infectious diseases.
Opportunities abound for medical device manufacturers to accelerate technology advancements in an effort to mitigate and reduce risks while keeping a keen eye on the top three critical factors: cost, comfort, and convenience. As the growing host of electronics continues to be added directly to plastic substrates, the value derived from the features such as flexibility, stretchability, low weight, and thin profile will go up.
Today, the immediate need is to accelerate the delivery of solutions that help mitigate risk and minimize cross-contamination transfer while continuing to provide superior quality of care to patients and protecting healthcare workers on the front lines. Ongoing technology advancements will likely spur a pivot to new fields, some of which may not exist right now. Opportunities to leverage printed and flexible hybrid electronics will serve as an essential springboard to major medical device breakthroughs and game-changing “low-touch” and “no-touch” applications.
The author would like to recognize the contributions of Jabil’s global team members, employees all over the world, and ecosystem partners that contribute towards the advancement of this technology during these unusual times.
About the Author(s)
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
