October 14, 2016
A new technique developed by researchers at MIT can test tumors for drug susceptibility by measuring how cancer drugs affect the growth rate of cancerous tumors in single cells.
Kristopher Sturgis
 When it comes to cancer treatment, selecting cancer drugs can oftentimes be a process of trial and error. There can be drugs that work for some patients that may not help others, while other drugs may be rendered ineffective by tumors that grow resistant. In an effort to help develop treatments tailored to individual patients, researchers from MIT and Dana-Farber Cancer Institute have created a novel method to test tumors for drug susceptibility through the use of a device that can measure the mass of a single cell--allowing researchers to predict whether a particular drug can kill tumor cells.
When it comes to cancer treatment, selecting cancer drugs can oftentimes be a process of trial and error. There can be drugs that work for some patients that may not help others, while other drugs may be rendered ineffective by tumors that grow resistant. In an effort to help develop treatments tailored to individual patients, researchers from MIT and Dana-Farber Cancer Institute have created a novel method to test tumors for drug susceptibility through the use of a device that can measure the mass of a single cell--allowing researchers to predict whether a particular drug can kill tumor cells.
The device, known as a suspended microchannel resonator, is essentially a functional assay designed to measure the drug response of individual cells. Mark Stevens, research scientist at the Dana-Farber Cancer Institute and lead author on the work, says the device was created in part to measure cell growth in the presence or absence of different drugs.
"The suspended microchannel resonator is essentially a tiny diving board that has a microfluidic channel running through it," he says. "Just like at a pool when a person is on the end of a diving board, it resonates up and down at a slower rate than when they jump off. Using this same principle at the micro-scale, we can measure single-cells with a precision of less than one ten-thousandth of their total buoyant mass. By taking many of these cantilevers, placing them along on a single path, and spacing measurements in time, we can measure mass accumulation over time--effectively the cell growth rate."
Stevens says that because their measurements take place in fluid, it's easy for them to measure cells in virtually any growth media or treatment condition, effectively allowing them to measure cells both in the presence or absence of a drug. While functional assays for cancer drugs have been around for decades, Stevens says their new method is quicker than most traditional methods and can produce accurate results with a very small number of cells.
"Functional assays to test the therapeutic susceptibility of cancer cells have been applied in the laboratory for more than half a century," he says. "However, many challenges exist when translating these assays to the clinic, driven by cancer biology. One of the biggest challenges is that primary cancer cells rarely proliferate ex vivo, meaning many traditional assays that depend on cell proliferation are not possible. The promising aspect of our assay is that we are able to measure single-cell mass accumulation in just 15 minutes. So with a relatively small number of single-cells, we can see whether cell mass accumulation is reduced when treated with a drug."
To test their new method, the team analyzed different subtypes of glioblastoma and leukemia cells that have previously been shown resistance to specific drug therapies. After exposing the cancer cells to these specific drug therapies, the group waited about 15 hours before measuring the cell's growth rates. They measured each cell several times over a 15 to 20 minute period to provide enough data to calculate the mass accumulation rate. What they found was that the cells known to be susceptible to a given therapy had altered the way they accumulated mass, while the resistant cells continued to grow unaffected.
Stevens was quick to note that the reliability and efficiency of this approach still remains unclear, as they expect certain subsets of diseases may be more amenable to this assay than others.
"Given the added complexity of human disease, answers to these questions would need to be carefully pursued in the setting of a clinical trial," he says. "However, given our assay's ability to probe single-cells, its compatibility with other assays, and relatively limited exposure to in vitro conditions, we feel that it has great promise to contribute to our understanding of cancer biology."
The group first reported their results in the October 10th issue of Nature Biotechnology, and they plan to continue their research in an effort to eventually formalize the assay into a clinical test that could one day potentially guide treatment decisions.
"The community of researchers pursuing novel functional assays is growing in size, and so is the enthusiasm for integrative metrics of identifying cancer cell drug susceptibility," Stevens says. "Additionally, these types of approaches are already being used with clinical samples to provide novel perspectives on therapeutic resistance in cancer--a necessary step to understand the breadth of their utility. Formalizing the assays into clinical tests that guide treatment decisions may take a decade or more, but hopefully the growing interest in these approaches from academics and industry can accelerate this timeline."
Kristopher Sturgis is a contributor to Qmed.
Like what you're reading? Subscribe to our daily e-newsletter.
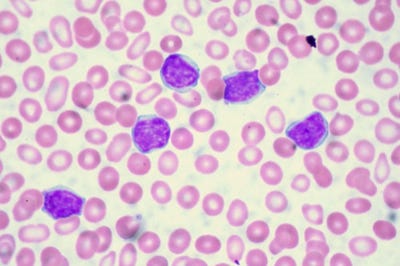
[Image courtesy of Ed Uthman/CC By-SA 3.0]
About the Author(s)
You May Also Like


