Why Flex Circuits and Tiny Batteries Are MedTech Game Changers
February 7, 2014
Think sensors galore and tinier, longer-lasting devices. A self-powered pacemaker might even be possible.
You say you want a revolution in medical devices? Then watch out, because recent breakthroughs in flexible electronics and battery technology could give you just that.
Such breakthroughs have the potential to enable applications ranging from self-powered pacemakers to edible medical devices. They're providing the most recent example of electronics advances once again begetting medical device advances.
Making Electronics Bendy
It is a simple problem--electronics baked on silicon chips are rigid and flat, while the human body is mostly curvy and flexible.
Researchers in recent years have figured out how to lift thin circuitry and other electronic components off the silicon chips they are baked on, embedding them instead on flexible materials that can fit along the contours of the body or a curvy medical device.
Flexible electronics technology pioneered by John Rogers, PhD, of the University of Illinois-Champaign, could enable an array of new medical devices that can conform to the uneven contours of the skin and internal organs. In addition, flexible electronics could be incorporated into existing medical devices to extend their functionality.
Rogers and colleagues spent years figuring out how to bake thin silicon circuits on a silicon base or substrate, chemically wash away the silicon surface underneath the circuit, and then use a specially designed rubber stamp to ever-so-gently transfer the thin circuit away to a flexible base.
Rogers thinks it is this transference process--this ability to remove circuits and other electrical components from the silicon they are baked on in a reasonable, reliable way--that is enabling all kinds of flexible electronic innovations such as body sensors that can be slapped onto the skin like a Band-Aid.
"It's opened up all kinds of new opportunities in using high performance materials in flexible formats. ... I think that's the difference compared to where people were in the past," Rogers says.
Some of the designs are already being commercialized by Cambridge, MA-based MC10, which Rogers co-founded.
Other pioneers include Michael McAlpine, an assistant professor of mechanical and aerospace engineering at Princeton University, who is experimenting with embedding flexible electronics in human body parts grown in the lab.
See Princeton University's John McAlpine discuss bionic nanomaterials on the Center State at MD&M West, February 10-13 in Anaheim, CA. |
Rogers acknowledges that flexible circuitry on implantable medical devices could be at least a decade away, due to the FDA's strenuous regulatory process.
"At the same time there are some opportunities to get the technology out sooner rather than later. We can have an impact in that way, and at the same time you can learn a lot about what type of designs are effective and which are not," Rogers says.
|
Discreet wellness sensors are among the products MC10 has been commercializing. (Image courtesy of MC10.) |
MC10 has physical sensors and diagnostic tools that stick onto the skin, and it is developing a balloon catheter with sensors embedded inside the actual balloon. Such a balloon catheter, for example, could take multiple readings at once inside a chamber of the heart.
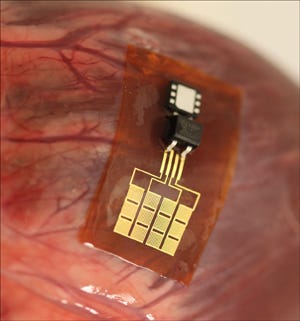
Rogers meanwhile continues to pioneer some pretty exotic implantable device ideas. He recently announced the creation of a super-thin silicone-encased, bendable energy harvester that can be affixed to a beating heart.
Rogers and colleagues have placed the device on the surface of hearts beating inside anesthetized cows and sheep, demonstrating that it can produce up to 1.2 ?W/cm², according to a paper Rogers and his colleagues recently published in the Proceedings of that National Academy of Sciences.
A millionth of a Watt is not a lot, but it is enough to power a pacemaker, Rogers says. Embed more flexible components inside the silicone, and it might even become a complete pacemaker.
Rogers and colleagues have placed the energy harvester on the surface of hearts beating inside anesthetized cows and sheep, demonstrating that it can produce enough electricity to power a pacemaker.
The energy harvester, though, still needs long-term trials to show it can hold up inside animals, Rogers acknowledges. Human trials could be a decade or more away in the United States.
Batteries inside some of the tiny, next-generation leadless pacemakers such as St. Jude Medical's Nanostim or Medtronic's Micra can last for 10 to 13 years, so the flexible electronics power generator will have to last even longer to be worthwhile, Rogers says.
|
Rogers and colleagues have placed a flexible energy harvester on the surface of hearts beating inside anesthetized cows and sheep, demonstrating that it can produce enough electricity to power a pacemaker. |
It has been a serious design challenge to get pacemaker and defibrillator leads to hold up inside the human body, so a constantly moving thin piece of thin ceramic would be even trickier, says Mir Imran, a medical device pioneer and electrical engineer who is CEO of San Jose, CA-based InCube Labs.
"Imagine, in a lead all you have are wires. It takes a lot of very clever design to keep them going for 20 years. How are you going to keep complex and ceramics from not cracking within a few days or months at most?" Imran says.
The energy harvester, for example, has been cycled 10 million times in a lab, but the human heart beats about 35 million times a year. Go for 10 years, and the device needs to cycle 350 million times.
"We understand that is just a start," Rogers says of the 10 million figure.
Imran suspects that disposable sensors are a better fit for flexible electronics. "I thinks that's where flexible electronics will go, is on the body."
Still, it is at least possible now that medical device designers will one day be able to power their creations using the natural movements of the patient using the device--including heartbeat-powered pacemakers and potentially defibrillators if flexible batteries are packaged in.
That could means much tinier, less-invasive devices for the hundreds of thousands of heart disease patients presently using pacemakers and defibrillators.
The challenges that Rogers and his research partners had to overcome over two and a half years demonstrate why it is only now that powering a device off a beating heart seems even remotely possible.
Rogers latched onto the idea of using a piezoelectric substance, a material that generates electricity when it is moved, to create an energy harvester. He ended up opting a crystalline, ceramic compound called lead zirconate titanate, called PZT for short, because it is already commonly used.
Three major challenges then occupied much of Rogers' and his colleagues time:
They needed to produce PZT layers that were actually flexible. The answer was similar to what Rogers latched onto for flexible silicon circuitry--make it really thin. PZT is also baked on a silicon substrate, so Rogers' team used similar methods to transfer it to the flexible silicone.
Power generation needed to be super efficient. A beating human heart only produces 2 to 3 Watts, and Rogers knew the energy harvester would only be able to harvest a tiny fraction of that if it was to avoid damaging the heart. These were PZT layers embedded in silicone and integrated with rectifiers and millimeter-scale batteries. Research partners at Northwestern University ran countless computer simulations to figure out the optimal layering of PZT that would produce the most energy.
It also needed to avoid damaging the heart. The more external pressure the energy harvester places on the heart, the more electricity it will produce. A good start was to make sure the energy producer put less pressure on the heart than the natural pericardium encasing it. Next were the open heart experiments on the live cows and sheep conducted at the University of Arizona. As a result of the experiments, Rogers suspects it is safe to produce a few microwatts off a beating heart, though not much more.
More electricity might be possible off lung movement, abdominal movements, or even muscle movement. But with the heart, a few microwatts is a safe range if designers are to avoid disrupting the beating of the heart, according to Rogers.
Building a Better Battery
Batteries meanwhile appear to be all the rage in Silicon Valley, with innovators taking note that many batteries still rely on a 20th century lithium-ion cocktail that has only improved incrementally over the decades.
While microprocessors have exponentially improved under Moore's Law, batteries have not increased in capabilities substantially, according to Imran.
"I'm always looking for new battery technologies," Imran says.
Learn about cutting-edge medtech technologies and trends at MD&M West, which is held February 10-13 in Anaheim, CA. |
The New York Times recently noted this trend, as well as the hurdles that come along with it:
"The problem, in part, is that it is hard to ensure the safety of many new power technologies. A faulty battery could potentially turn into a miniature bomb. So the products require exhaustive testing by regulators before hitting store shelves. Even if a new power system is approved, it often requires adoption by reputable brands like Apple, Samsung, or Microsoft before everyday consumers start to trust it."
There are some major research breakthroughs, however, that are worth taking note of--improvements that could enable a whole host of new medical devices.
Here are three ways batteries are improving:
They're becoming edible. Imran has InCube engaging in its own research in the area. There has been plenty of interest in ingestible medical devices that might release medications in a systematic way or use cameras to scope out the digestive tract. A usable edible battery would allow for such devices to simply break up in the digestive tract, and whatever came out the other end would be environmentally friendly.
Carnegie Mellon University's Chris Bettinger and Jay Whitacre have latched onto cuttlefish ink as a possibility for this application. The two researchers had already reported some success creating edible power sources using materials found in a daily diet. But they still needed to find the optimal pigment-based anodes to include in their edible sodium-ion batteries. They ended up finding out that naturally occurring melanins derived from cuttlefish ink exhibit higher charge storage capacity compared to other synthetic melanin derivatives when used as anode materials.
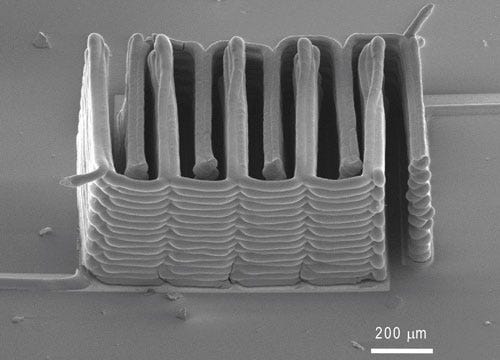
They're getting tinier. Researchers based at Harvard University and the University of Illinois at Urbana-Champaign have figured out how to 3-D print microbatteries only 1 mm in width. Tiny batteries are revolutionary because this is about producing the electronic guts of what goes into a medical device. The tinier the battery, the tinier the device.
A research team led by Harvard engineering professor Jennifer Lewis have created and tested materials, or "inks," able to function as electrochemically active materials. The materials had to harden into layers in just the right way so they could be stacked up in layers during the 3-D printing--creating working anodes and cathodes. The researchers say their tiny batteries have electrochemical performance is comparable to commercial batteries in terms of charge and discharge rate.
|
Researchers used 3-D printing to create an interlaced stack of electrodes layer by layer, producing the working anode and cathode of a microbattery. (Image courtesy of Harvard University, Jennifer Lewis) |
Besides tiny, flexible is another option. Researchers at Northwestern University and the University of Illinois, including Rogers, have been working on flexible batteries that would be compatible with stretchable electronics. The batteries could be used inside of or on the body to power a variety of medical devices. The batteries can be stretched up to 300% of their original size and be recharged wirelessly.
They can be charged through the air.A team of physicists at the Massachusetts Institute of Technology in 2007 came up with a scheme for manipulating magnetic fields in order to transfer energy over a distance, and even through body tissue to a medical device.
Medical device designers have already latched onto the technology as they work on next-generation pacemakers and left ventricular assist devices, because it would be a huge improvement to avoid running wires through the skin or operating to change a battery.
Wireless battery charging technology appears to be improving even more.
The New York Times reports that Apple is actually testing using magnetic induction to charge its iWatch under development: "A similar technology is already used in some Nokia smartphones -- when a phone is placed on a charging plate, an electrical current creates a magnetic field, which creates voltage that powers the phone."
According to MacRumours, the iWatch could recharge its "rumored 100mAh battery [...] from up to a meter away."
Chris Newmarker is senior editor of MPMN and Qmed. Follow him on Twitter at @newmarker and Google+.
About the Author(s)
You May Also Like


.png?width=300&auto=webp&quality=80&disable=upscale)
