Artificial Pancreas, Injection Sites, and Fast-Acting Insulin: Diabetes Trends and Challenges
Bill Betten recently attended the 5th International Advanced Technologies and Treatments for Diabetes (yep, the poor guy just had to go to Barcelona).
February 28, 2012
Bill  Betten recently attended the 5th International Advanced Technologies and Treatments for Diabetes (yep, the poor guy just had to go to Barcelona). Afterwards, he was kind enough to provide MD+DI with his observations from the event, highlighting trends in the sector.
Betten recently attended the 5th International Advanced Technologies and Treatments for Diabetes (yep, the poor guy just had to go to Barcelona). Afterwards, he was kind enough to provide MD+DI with his observations from the event, highlighting trends in the sector.
What were some diabetes trends that you noticed?
A keynote talk was given on “What Next for Diabetes Technology: Strategic Directions for the Next 10 Years,” by J. Pickup of London. The five highlighted buzzwords included cost effectiveness, nanomedicine, mobile health, optical sensing, and closed-loop insulin delivery. A point that he made is that insulin pumps, for example, have taken over 30 years to reach maturity, and continuous glucose monitors (GCMs) have been around since 1999 and are not yet beyond clinical trials. Even with insulin pumps, a lot of discussion was around a low glucose suspend (LGS) mode of operation, which allowed the pump to stop infusing insulin for up to a two-hour period as a mechanism for avoiding hypoglycemia. Apparently this mode is controversial enough that it is not yet approved in the United States. If this isn’t possible, then the prospect of going completely closed loop is still out in the future.
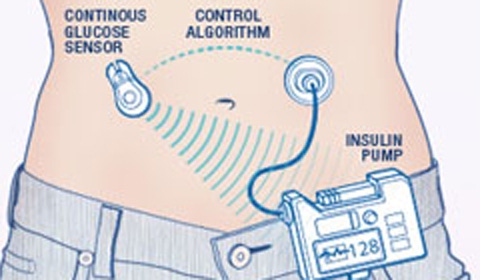
Many of the presentations centered around closed-loop monitoring of insulin patients, up to and including the creation of an artificial pancreas. Fundamental elements of closed loop systems are the sensors, a processing board with signal processing, an insulin pump, and a delivery mechanism for the insulin into the body.
Can you tell me more about the artificial pancreas technology?
There were a number of discussions associated with the creation of an artificial pancreas. In fact, there is a European sponsored project to focus on development of such a system. Common hardware configurations included the Dexcom Seven Plus CGM system plus an Insulet Omnipod pump. In between were a number of discussions about the hardware and signal processing designed to manage the entire loop. There were discussions about fuzzy logic, neural nets, and all kinds of management techniques designed to address the issues associated with closing the loop. At a very basic level the goal of such a system is to maintain the blood glucose level within an acceptable level (typically 70 – 140 mg/dL) while dealing with the disruptions of meals and physical activity. While this might seem to be a classical feedback control-loop problem, the difficulties start with the inaccuracy of the continuous glucose monitoring (CGM) sensor and relating that to actual glucose in the bloodstream. The difficulties continue with the lag times of insulin injection, impact on the body, and duration of the insulin in the blood stream. It is like trying to hit a moving target while the background conditions are continually changing. Draft guidelines exist from the US FDA and can serve as a framework for investigations into this area.
What are some other challenges to managing and treating diabetes?
The choice of site for injection of insulin is clearly an issue, given the different physiology of the body and how it takes the insulin into the blood stream. Injection into the subcutaneous tissue can have a different reaction time than deeper within the body. One of the key targets for insulin pumps is to keep a minimum dosing levels running as a background, and then using a larger bolus injection to address meals, exercise, etc.
A very definite need is faster acting insulin with shorter duration in the body. Numerous fast-acting versions exist, but long-term persistence remains an issue, increasing the risk associated with hypoglycemia (low blood sugar). The risks associated with hypoglycemia are short term from the perspective that too low of a blood sugar can cause a coma and death quickly (less than an hour), while the effects of hyperglycemia (high blood sugar) tend to be long term due to impact on blood vessels (nerve damage, poor circulation, loss of eyesight, potential amputation, etc.). Either condition is serious, but the emphasis is on prevention of hypoglycemia since it has more immediate consequences. In addition, inhaled insulin is being assessed as an alternative or enhanced method of delivery of the drug.
A critical aspect of both the measurement of blood glucose levels is the sampling location. The most representative sampling method is directly from the blood, hence the popularity of the blood glucose measurement sticks. The continuous glucose monitors sense the glucose in the interstitial layers underneath the skin, which is different than the level in the blood. Other methods, including optical, are being explored, but none of these seem to be acceptable yet.
Better sensors are required due to relatively poor accuracy, particularly in CGM, and need for increased reliability. The margin of error with CGM sensors is sufficiently broad that they must be calibrated via a blood stick typically at least every 12 hours and cannot currently be used for long term closed loop patient treatment.
 Were there any particular devices that caught your attention?
Were there any particular devices that caught your attention?

There was much discussion around the Roche Diaport system. Basically this is a port implanted in the body that allows connection to the insulin pump system. However, a key attribute of this system seems to be the placement of the catheter into a deeper portion of the body, nearer to the liver, to enhance the take up of the insulin into the body. One of the problems with injection of the insulin into the body as well can be adhesion and overgrowth along the injection site, limiting the ability to keep the site open and necessitating relocation of the injection location. The Diaport catheter is apparently designed to float within the abdomen and help allay such problems. In addition, there were discussions of injection of another drug with the insulin to facilitate the injection location’s ability to take up insulin as well as using a heating mechanism to do this as well.
—Heather Thompson
Further Reading
Product Teardown: Inside the Dexcom Seven Plus Continuous Glucose Monitoring System
Tech Review: JDRF’s Insulin Initiative: Afrezza, Roche’s DiaPort, Smart Insulin and More
Patient Perspectives: Tom Brobson: My Experience in the Artificial Pancreas Clinical Trials
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
