Hospitals Don’t Pass Supply Chain Discounts to Patients
The reason healthcare costs are increasing is not due to the rising expense of medical devices and treatments; it’s due to double-digit increases in chargemaster prices.
June 12, 2015

The reason healthcare costs are increasing is not due to the rising expense of medical devices and treatments; it’s due to double-digit increases in chargemaster prices.
Steve Reilly
I recently attended a symposium with a panel of hospital system executives. The topics ranged from improving patient care to the impact of the Affordable Care Act on hospital finances.
In one of the question-and-answer sessions, a hospital system CEO was asked about the impact of Medicare’s value-based contracting on his hospital system’s revenues and profits.
|
Reilly |
His response, “Well, as you know, the value-based contracting can reduce hospital revenues by as much as 1.5% per year. My system has annual patient revenues of more than $3 billion, so even 1.5% is a very big number.”
Unfortunately for him, I have much more information on the structure and incentives of value-based contracting than the average person. I raised my hand.
“As I understand it, Medicare’s value-based contracting incentives only apply to Medicare and Medicaid patients, is that right?” I asked.
“Well, yes,” the CEO replied.
“So that would mean the 1.5% penalty only applies to the CMS side of the reimbursement equation,” I said. “Which would mean reimbursement from the private payers is not penalized in any way. Correct?”
“Ah… that would be correct,” he replied.
“Also, as I understand it, the ‘penalty’ of a 1.5% reduction in CMS payments only applies in full if your hospitals or hospital systems fall below the 50th percentile in comparison with other hospitals,” I said. “Isn’t that also correct, sir?”
“Yes, you are correct,” he replied.
“So wouldn’t it would be more correct to say that your hospital and hospital system might be penalized up to 1.5% by CMS on CMS payments only if you do not meet your quality metrics?” I asked.
“Uh, yes,” the CEO replied.
“And according to CMS, Medicare and Medicaid raised their payments to hospitals by more than 2% in 2015. Is that also true?” I asked.
He paused for a minute, and then asked, “Who are you?”
“Just an informed healthcare consumer, sir,” I said.
Every day I listen to hospitals claim they need to cut costs because Medicare is reducing their reimbursement. They use this false argument (i.e., lie) as a negotiation ploy to get medical suppliers to lower their prices. That’s not necessarily a bad thing; it is always better to have lower prices than higher prices. But what bothers me is that they then use these widened profitability margins to increase executive salaries and invest in larger and nicer hospital campuses and buildings. The cost reductions hospitals manage to wrangle from their suppliers are not passed on to patients or used to decrease patients’ costs in any way.
Here are the facts. Medicare increased hospital payments by 2.1% across the board in 2015, and the decreases due to value-based contracting were less than 0.2% in aggregate. In fact, hospitals continue to increase their profitability at alarming rates and much faster than the rest of the U.S. economy.
How do they do this?
The main vehicle used by hospitals to increase their already huge profit margins is the chargemaster or charge description master (CDM) list. The chargemaster has gotten quite a bit of (but not nearly enough) press with the publication of Yale Professor Steven Brill’s treatise on hospital overcharging in Time magazine, titled A Bitter Pill.
In response, hospitals claim the CDM is irrelevant to hospital inflation for a couple of reasons.
Specious argument No. 1: No one actually pays Chargemaster prices.
It is true that very few patients actually end up paying the grossly inflated charges generated on a hospital bill, with the exception of foreign patients who come here to have surgery. (This week, the person in charge of international transplant marketing for a major health system told me that the negotiated rate with foreign embassies for foreign patients is usually 100% of charges. He also said that his hospital marks up the organs used in transplant operations by as much as 700%. A kidney procured by a hospital for $30,000 can be “resold” to a patient for more that $100,000. Talk about socking it to the sick!)
The other patient populations paying chargemaster prices are those least likely to be able to pay, the uninsured. Hospital billing and collection departments chase down nonpaying customers for reimbursement at chargemaster rates. Some even hire collection agencies to chase uninsured patients, forcing people into bankruptcies or worse. Hospitals will tell you that they usually settle for something less than billed charges, but 100% of billed charges (at some hospitals this can be 1300% of the actual cost) are where the negotiations begin.
Specious Argument No. 2: Nobody pays attention to chargemaster because it is irrelevant to hospital profitability.
The argument that because hospital chargemaster numbers are so inflated, no one takes them seriously, is a joke. First of all, my private insurance clients, including Blue Cross and United HealthCare, continually struggle to negotiate hospital contracts that do not rely on a percent of charge (CDM) payment methodology. If they are not successful, they at least try to include contract terms that limit the amount a hospital can increase its charges to less than 10% per year.
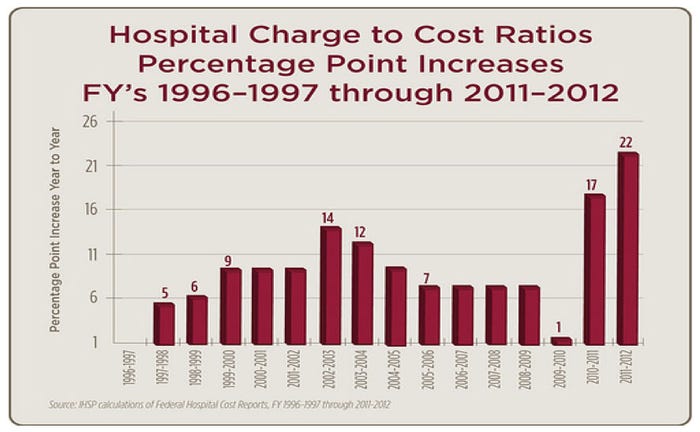
Figure 1. One way hospitals can increase revenue.
Figure 1 illustrates how hospitals use the chargemaster as a tool to increase revenue. Prior to the introduction of the ACA, hospitals were gradually reducing the amount of increases to their CDMs. But when faced with the uncertain environment of hospital revenue under the ACA, they decided to err on the side of gross—truly gross—profits by increasing patient charges by double digits. Figure 1 shows that hospitals in aggregate increased their chargemaster pricing by 17% in 2011 and 22% in 2012. (In both those years, inflation was less than 2%.) Since this information was made public, hospitals have stopped reporting their chargemaster numbers in every state with the exception of California.
Now, I am an American and a confirmed capitalist, but this is unconscionable for two reasons.
First, even though health insurance plans try to keep hospital Chargemaster prices under control, they don’t do this for socially conscious reasons. They do this to improve their own bottom lines. Ultimately, they all pass the increased costs to consumers in the form of premiums. In the end, it is the patient who suffers, not the insurance company.
Second, not only are hospitals increasing their revenue, they are also reducing their charitable care for communities. The tax benefits these hospitals receive from their “nonprofit” status actually reduces the amount of social services that could be delivered to those in need if these health systems paid local taxes. Sixty percent of U.S. hospitals are designated as nonprofit. To achieve and maintain this status, the hospitals must spend at least 3% of their operating revenue on charitable care, including taking care of uninsured patients. Many hospitals are noncompliant and some spend as little as 0.7% on charitable care (and these “unrecoverable” charges are at CDM prices that are hugely inflated from actual costs).
In the end, the reason healthcare costs are increasing as much as they have is not due to the rising expense of medical devices and treatments; it’s due to the indefensible double-digit increases in chargemaster prices. And if you wonder how it is possible for hospital executives to sleep at night with this kind of patient gouging, you can be sure they sleep comfortably . . . on large sacks of money.
Steve Reilly can be reached at [email protected].
[main image courtesy of VICHAYA KIATYING-ANGSULEE/FREEDIGITALPHOTOS.NET]
You May Also Like



