Desktop 3-D Printer Takes on Infections and Cancer
May 12, 2015
Researchers at Louisiana Tech are using an inexpensive 3-D printer to make novel medical implants.
Brian Buntz
|
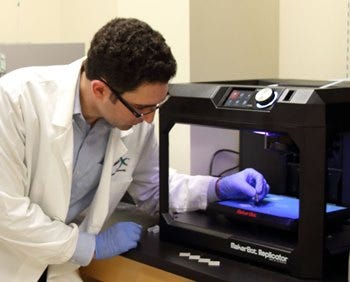
Louisiana Tech doctoral student Jeffery Weisman uses a MakerBot 3-D printer to create antibacterial beads. |
The MakerBot line of 3-D printers are slick. The printers have won a slew of awards including a variety of CES prizes. A MakerBot was named one of the best inventions of 2012 by Time magazine, the overall winner in the 3-D printing category and product of the year in Popular Mechanics. The devices also happens to be inexpensive for a 3-D printer; the least expensive MakerBot device can be had for around $1300.00.
It was only a matter of time before someone decided to use MakerBot technology for medical applications. One of the first groups to do so were researchers from Louisiana Tech University (Ruston, LA). They used the MakerBot 3-D printer and extruders from ExtrusionBot to create custom medical implants out of resorbable plastics. That accomplishment is especially impressive considering that, in the past, embedding additives in plastic required industrial-scale equipment to guarantee that the materials within the extruded plastic were evenly dispersed.
Led by David K. Mills, PhD, a professor of biological sciences and biomedical engineering at the university and Jeffery Weisman, PhD, a research associate working with Mills, the research group is using what it what it terms nanoenhanced materials to create multifunctional implants. (Mills and Weisman are speaking on the subject of 3-D printed biocompatible nanotechnologies at MD&M East on June 11.)
One example of such an application is an improved version of antibiotic beads, which are used to treat chronic wounds and other problems. Antibiotic-coated poly(methylmethacrylate) (PMMA) glass beads, resembling a string of pearls, have been used for years in surgery. Made of Plexiglas, they are placed in a wound and wound site sutured back up. The antibiotic it contains is gradually released and that hopefully controls the infection.
Mills will be speaking at MD&M East on June 11. |
"The problem is that, in most cases, the glass beads can only provide one antibiotic. If you are dealing with a very traumatic wound--a car crash, battlefield injury--in many cases, you may find there are a number of different bacterial vectors that have colonized that wound. So you may really need multiple antibiotics," Mills says. "Second, the surgeon has to go in after a period of time, because the beads are not resorbable, and remove them." A secondary surgery carries with it an added risk of infection.
"The other liability is that the surgeon can never really be sure how much antibiotic is being delivered. It is usually necessary to supplement that with systemic--a drip or alternatively a big antibiotic pill," Mills notes.
Mils and his team at Louisiana Tech have come up with a resorbable bead that can be loaded with a variety of antibiotics and antifungals. "Since they break down in the body, in most cases, they end up as lactic acid. And there is no additional surgery," he explains.
The resorbable beads are partly hollow, which enables the researchers to optimize the beads' drug delivery profile thanks to the beads' increased surface area.
The ability to avoid a second surgery could be especially useful for frail patients, for whom a repeat surgery could be more harmful than simply trying to control the infection.
The Louisiana Tech researchers are also using biomedical devices that elute chemotherapeutics. "The key feature there is that we are using nanoparticle to enhance or add new capabilities to those materials for targeted drug delivery. The phrase we like to use is 'local and focal,'" Mills says. "It is a localized delivery instead of being system. And second, it is a focal load as opposed to being a systemic load. A systemic load leads to a lot of side effects from loss of appetite, loss of hair, problems with the immune system, etc."
The researchers' approach differs from others in the sense that the delivery system is unique. "In some case, we would be incorporating our material directly into surgical materials that would be applied to the surgical site after tumor resection," Mills says.
Other researchers have used nanoparticles with a targeting system to ferry a drug to a tumor site.
"We are developing materials that the surgeon would use during and then after tumor resections or applied directly to the affected site as opposed to using the blood stream as a way of getting nanoparticles there," Mills says.
Check out Mills and Weisman's talk at MD&M East in New York City, June 9-11, 2015. |
Like what you're reading? Subscribe to our daily e-newsletter.
About the Author(s)
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
