FDA's Final UDI Rule: A Few Tricks But Mostly Treats
The final rule for unique device identification is mostly favorable to industry, but some provisions of the rule could be challenging to implement.
October 4, 2013
On September 24, 2013, FDA published its final rule for a system of Unique Device Identification (UDI). The rule has been a few years coming, so industry insiders that had time to get intimate with earlier drafts of the rule likely let out a sigh of relief when they saw the final version.
Don't miss the conference session on "The Next Steps in UDI Implementation," presented by GS1's M.J. Wylie, at MD&M Minneapolis on October 28, 2013. |
The core framework for the final UDI rule is mostly unchanged from the proposed rule published earlier this year:
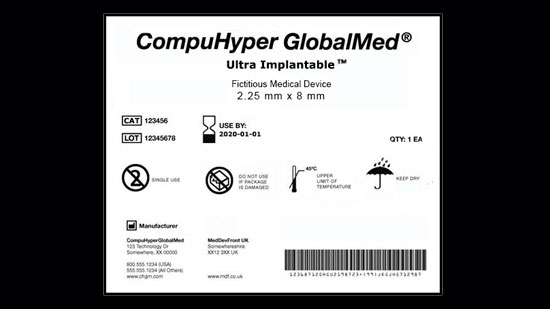
Labels. As a general rule, all product labels for medical devices must bear a UDI—a combination of a device identifier and a production identifier—in both a human-readable form and a machine-readable form, using Automatic Identification and Data Capture (AIDC technology). All other special exceptions and exemptions, where UDIs may not be required, are exceptions to the general rule.
Database. Product data for all medical devices must be submitted and kept up to date in an FDA-managed Global Unique Device Identification Database (GUDID).
Direct Marking. The device identifier must be directly marked on certain categories of devices.
Timeline. Compliance dates take effect over time using a risk-based approach. For example, labeling and GUDID submission requirements are phased in by device class over a five-year period, while direct marking compliance requirements are phased in over a seven-year period.
Beyond the core rule, however, FDA listened to feedback from industry and incorporated a number of meaningful changes to its original proposal. The final rule strikes a good balance of common sense and public safety without overly burdening the industry.
The Treats
Taken as a whole, the changes made to the final UDI rule were mostly favorable to industry. But that’s not to say they were giveaways. In most cases, the modifications were a result of legitimate industry concerns—a provision was too burdensome, was inconsistent with other regulations, would not improve public safety, or some combination of the above.
Here’s a look at some of the changes and how they benefit industry:
FINAL RULE | ANALYSIS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The Tricks
There really were not any crazy new tricks added to the final rule that would have caught the industry off guard. The following provisions, however, will be trickier than others to implement:
FINAL RULE | ANALYSIS |
|
|
|
|
|
|
|
|
The Final UDI Rule is Good for the Industry
FDA senior advisor for patient safety Jay Crowley and his team raised a glass of sparkling cider to industry attendees at the FDA UDI Conference in Baltimore on the morning of September 24, 2013, when they announced that the final rule had been accepted. We believe the industry is right to raise a glass to toast the arrival of the final rule. Now that we all know what that target is we are working toward—and that target looks pretty reasonable—companies can get on with the business of assessing gaps in their own UDI program and developing an implementation plan that will bring them to a state of UDI compliance. After that, the future holds many opportunities for additional longer-term benefits from UDI.
Learn more about how to implement UDI at the MD&M Minneapolis conference. |
Cathi Crist is a partner with Kalypso. Scott Gibbard is a senior manager.
[image courtesy of FDA]
You May Also Like

