Breathing New Life into Biomaterials
December 15, 2014
Material scientists are learning to program biomaterials, giving them the ability to better interface with the body.
We have smartphones. Why not smart biomaterials?
In a way, traditional materials destined for use within the body are like the phones from yesteryear: good for a single purpose and not much else (though they do last for decades).
In the past, the best biomaterials were thought to be as inert and stable as possible; the best possible outcome for a biomaterial was to be ignored by the body. The reason for that aim was clear: biomaterial degradation was often linked to medical device failure.
Now, however, designer biomaterials are being devised that can either interface with the body or dissolve, leaving the body to remodel the tissue as it breaks down. "You have a lot of little levers to tweak, and those levers are all levers in organic chemistry," says Walter E. Voit, PhD, an assistant professor of materials science and engineering at the University of Texas at Dallas.
In addition to breakthroughs in material science, advances in implantable bioelectronics, 3-D printing, and computer processing have also changed the game.
Material scientists are not only tweaking how they make polymers and how those polymers are linked together, but also how they interface electronics, semiconductors into layers into those materials, according to Voit.
"The tools of today allow us to do that with far greater precision than what could have been done 20 or 30 years ago," says Voit, whose group has received funding support from GlaxoSmithKline.
One example of what Voit is describing is the use of dissolvable thiolene/acrylates-based substrate to house flexible biocompatible electronics (such as gold) within. Those electronics can be used to interact with nerve bundles only 60 microns in diameter, or even tinier nerve fibers. Such electronics cannot be sealed off from the body in the same manner as, say, a pacemaker is with a metal can, Voit says. In fact, it helps to have them degrade in a controlled way so that cells from the body can grow in and create a better, safer interface.
"You have these giant devices that we want to interact with very, very small nerves. It becomes a size-distance problem. It would be great if we could design tiny components that are themselves well-encapsulated enough to prevent long-term disruption from the body but still interact with the body in controlled ways," Voit says.
Over the years, material scientists have worked on a variety of synthetic materials that degrade in the body in a controlled manner. The first notable example of this was the debut of the first polyglycolide sutures in the 1960s, which gradually dissolved, eliminating the need of a physician to remove them later.
Until recent years, though, Voit could only count a handful of degradable materials included in FDA master files. But that is gradually changing, and biodegradable implants are in ever-greater demand.
A new world of hacking biomaterials has arrived.
Programming Degradation
A major focus of Voit's research has involved shape-shifting thiolene/acrylates that could open the door for a whole new host of applications in medtech. The substance could enable self-coiling cochlear implants inside the ear, the aforementioned electrodes that can coil around a nerve, and a host of cardiovascular implants.
Voit is still engaged in preclinical trials with animals with the technology. He has financial backers including the Defense Advanced Research Projects Agency, GlaxoSmithKline, and Texas Instruments.
3M Co. undertook research on thiol-type polymers in the late 1970s but did not commmercialize this likely because computers at the time were not available to handle the data rates that now make these devices useful, Voit says. In addition, poor shelf life of the materials restricted their commercial applications. Only in recent years have researchers begun to capitalize on the thiol-type polymers' ability to soften and change shape under human body temperatures for promising potential commercial applications. A polymer for example could be engineered to coil around nerve inside the human body.
Another aspect of the polymers that can be controlled is degradation, based on placement of ester-based substrates. Such controlled degradation could be useful in a number of ways.
For example, the shape-shifting polymers could be used to place electronics where they are needed--such as coiled around a nerve, and then the polymers could degrade away, leaving the electronics in place.
"It could give you a really nice controlled integration of biological tissue onto devices. If we can control how the body responds to devices, that allows us to control a lot better the electrical functionality of these devices," Voit says.
Another area of Voit's research involves silyl ether thiol-ene networks, which Voit has found can degrade within 30 minutes. Voit sees potential for such materials to be drug-delivery vehicles.
Toughening Up Biomaterials
One limitation of many resorbable biomaterials is their strength profile. While offering considerable strength upfront, their durability degrades quickly over time.
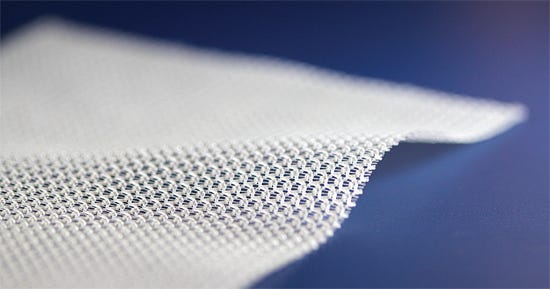
One company, Novus Scientific, sought to solve this problem through a material innovation that involved knitting two degradable polymers together to create a surgical mesh that provides tissue support for six to nine months.
The first of the two polymers, a copolymer of glycolide, lactide, and trimethylene carbonate (TMC), was engineered for fast resorption, offering mechanical strength for two months. The second, a copolymer of lactide and TMC, maintains mechanical strength for six to nine months. The mesh material completely degrades within three years.
|
Launched in the United States in 2010, the TIGR mesh is billed as the only long-term absorbable mesh. |
On the market internationally, the TIGR Matrix is being employed for abdominal wall repair and hernia prevention. "That is why, in this case, it holds the abdominal wall together for that six to nine months. ... A healthy person needs six months to recover after a surgery involving the abdominal wall," says Stefan Sowa, vice president operations and site manager at Novus Scientific's Uppsala, Sweden headquarters.
The quick-dissolving fiber offers strength initially after implantation. "In the first period, it keeps the tissue fixated very tightly. It is stiff," Sowa says. "Once the first type of fiber dissolves, you are left with the more elastic mesh."
This variable strength and elasticity profile assists the body in healing itself, according to the company. "One of the challenges with anything resorbable is what is left behind," says Tac-Whei Ong, president of Novus Scientific Inc.'s U.S. subsidiary, based in San Diego. "What is going to support this tissue from reherniating again?" he asks.
Several years ago, biologic mesh was hailed as a promising new treatment for applications including hernia repair, Ong says. "But those products failed in terms of remodeling," he says. In addition, biological mesh tends to cost considerably more than synthetic mesh.
It is also problematic to use metal-based mesh for hernia repair. "If you are looking at strength alone, titanium is the strongest material you could use," Ong says. "Titanium-based mesh failed miserably when used for this application." The abdominal wall is constantly moving, and inserting a stiff metallic mesh there can cause the tissue surrounding it to rip away.
So how does the TIGR mesh overcome these problems? It is designed to offer dynamic load transfer to the surrounding tissue, helping to spur healthy connective tissue growth rather than scar tissue.
The knitted material offers support while also stretching dynamically as the body's natural tissue does. "This allows the surrounding tissue to be trained to be remodeled," Ong says.
The body, after all, responds to load. Muscles and bone that are unused atrophy. Consider how astronauts in space lose bone and muscle mass, for instance.
TIGR was developed to respond to mechanical transduction. "Within the fibers of the collagen, there is this actin fibers that respond to load. As it responds to load as you move, it aligns collagen in the direction of the force," Ong says. "This is active mechanical remodeling." This leads the body to develop type-1 collagen, which is functional connective tissue, rather than type-3 collagen, which is scar tissue.
The company is broadening the scope of applications for the material beyond hernia reconstruction, and the material is now used in breast surgery as well.
The company is also open to selling the material to medical device companies on a license basis. "Anyone who wants a new indication would have to do a study so that it can be registered for that application with the appropriate regulatory body," says Stefan Sowa, vice president of operations and site manager in Sweden (Uppsala, Sweden). "But we are open to sublicensing--for instance, doing it for knees or something like that."
Finding Material Marriages of Convenience
Researchers at the Fraunhofer Institute for Manufacturing Technology and Advanced Materials in Bremen, Germany are working to develop a strong biodegradable biomaterial of a different sort: a metal-ceramic composites strong enough to be used as suture anchors to treat tendon rupture.
While traditional suture anchors succeed in holding torn tendons in place, the implants, which are made of titanium or an inert polymer, either remain permanently in the body after the tendon has healed or they are retrieved surgically.
Similar to the aforementioned example with the TIGR mesh, biodegradable tissue anchors must offer sufficient strength over the relatively long term. Fraunhofer researchers employed a similar strategy, too, using two materials with different degradation speeds. Iron alloys were used to corrode slowly, ensuring high mechanical strength while tricalcium phosphate (TCP) ceramic decomposes quickly, and can stimulate bone growth while aiding the ingrowth of the implant.
The Fraunhofer researchers used powder injection molding to create the components. This process offers the ability to produce complex structures cost-effectively and in large numbers. It also allows for properties such as density and porosity to be controlled selectively, which is crucial when developing materials with high mechanical strengths.
In addition to improving how some shoulder surgeries are performed, the underlying materials and manufacturing technology used to make the tissue anchors could serve as a building block for other biodegradable implants as well.
The German researchers plan to continue exploring how these materials react within the body.
About the Author(s)
You May Also Like