Designing Joint Implants That Enhance Patient Satisfaction
Here's how custom 3-D printing, porous metals, and innovative biomaterials are transforming knee and hip joint replacements.
July 15, 2016

Wendy Lyons Sunshine
This knee CT scan is an important part of the ConforMIS iFIT Image-to-Implant process. A 3-D model based on the scan image is used to build customized implants.
Board certified orthopaedic surgeon Gregory M. Martin, MD performs more total knee replacements than any other operation at his Boynton Beach, Florida, practice. Over the years, he began to realize he could do a great job in surgery, make cuts properly, insert implants properly, and have everything look great, with perfect X rays--and still have an unhappy patient.
"The studies are real," he said. "I see it in my own patients all week long and in the second opinions I give: patients who have had total knee replacements tell me they wonder why they did it. Their knees still hurt, it didn't meet their expectations; they say they felt better before surgery."
With over one million patients undergoing total hip and knee replacements in the U.S. each year, patient satisfaction has become a significant issue. What's more, data from the American Academy of Orthopaedic Surgeons (AAOS) indicates that patients electing total joint replacement are getting younger, too. Today, those who undergo the procedure are nearly as likely to be under the age of 65 years old as over it.
Younger patients heal faster than their older counterparts, but they are more likely to outlast their medical devices and require a second, revision surgery. Their active lifestyle puts extra strain on implants and cement fixatives. These factors compound the typical post-operative risks of joint squeaking, pain, infection, inflammation, and implant rejection.
In hopes of improving satisfaction and outcomes for his patient base, Martin decided to use ConforMIS' entirely customized joint replacement system. "It was a decision I made, and a shift for me," he said. With ConforMIS, the entire process is individualized based on the patient's CT scans: using 3D printing technology, jigs and cuts are individualized along with the actual implant size and shape.
Martin is on the ConforMIS advisory board and has been using that system ever since the device received FDA approval. Studies presented at conferences have cited a 92% patient satisfaction with ConforMIS, while published studies have found traditional systems earn satisfaction rates of 82-89%.
"Anecdotally, what I have seen in my practice is consistent patient satisfaction rates in upwards of 90% range," said Martin. "We've seen a dramatic reduction in blood loss, a reduction in length of stay, patients going home more often than going to rehab (including simultaneous bilateral knee replacements going home), and we've seen reduction in adverse events and improvement in overall satisfaction rates."
|
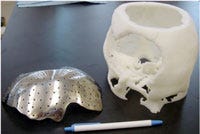
An example of 3-D printed patient-matched implants. |
To further enhance outcomes for patients, next-generation joint replacement systems could combine the just-in-time manufacturing flexibility of 3D printing with nano-scale materials and biodelivery of medications. At Washington State University, husband and wife researchers Amit Bandyopadhyay, PhD, and Susmita Bose, PhD, have invented 3-D printed porous metals and resorbable ceramic compositions specifically for bone engineering. With a $1.8 million NIH grant, their teams are working to create new joint replacement materials that promote patients' healing, reduce adverse reactions, and extend the life of implants.
Bose said that when an original implant needs to be replaced, currently no later than 10-15 years, the bone is typically very compromised and the second surgery is challenging. "After their second surgery, the bone is so compromised the surgery can't be repeated," said Bose. "If the surgery fails, the patient is wheel chair bound." This is a serious concern for younger patients who could easily live to 80 years or beyond. Her team is developing coated implants that improve bone bonding, which will be especially beneficial for revision surgeries. The coatings also include antimicrobials and antibiotics to control infection and control the biochemistry for surrounding tissue.
Under a National Science Foundation grant, Bandyopadhyay and Bose are also exploring alternatives to the CoCrMo alloy (containing cobalt, which has been linked to adverse reactions) that is commonly used in many load-bearing implant applications. "And, yes, we are using 3-D printing for that as well," said Bandyopadhyay.
The researchers recently co-authored a study in the Journal of the Mechanical Behavior of Biomedical Materials with a biomaterials engineer from Zimmer Biomet about reducing material loss and harmful metal ion release while simultaneously increasing wear resistance of arthroplasty implants using calcium phosphate (CaP)- titanium (Ti) composites.
Coated implants take longer to heal, but offer long-term benefits. Uncoated implants offer faster recovery times, but the cement used to secure them has a high rate of cracking.
"Today the patient takes a minimum of six weeks to six months before they can really get back to normal life," said Bandyopadhyay. "Our number one goal is to reduce the healing time, so patient comfort level is better."
"We're seeing a big shift toward a patient centered approach," observed Martin, "not only in knee replacements, but throughout healthcare--really looking at the end user and asking did they get quality and value for what was provided."
Wendy Lyons Sunshine is a freelance contributor to MD+DI. Reach her at [email protected].
[Top image courtesy of CONFORMIS. Second image courtesy of AMIT BANDYOPADHYAY and SUSMITA BOSE.]
You May Also Like