Unlocking the Power of Coronary CT Angiography
|
iSTOCKPHOTO |
There may be an opportunity for CT angiography to be used as an inexpensive screening tool to bring a large unidentified population with coronary artery disease (CAD) under medical surveillance—a population that would otherwise be susceptible to unexpected heart attack deaths. To harness this diagnostic tool, several other things need to happen: CT scanner speeds need to be increased to render the coronary artery blockages and calcifications conspicuous, radiation exposure needs to be further reduced, and the software behind this tool needs to be made more user-friendly and intuitive, i.e., capable of shutting the system down if radiation levels reach unsafe levels. Computer-aided diagnostic software, which uses pattern-recognition algorithms, could help improve the accuracy and specificity of identifying early coronary vessel calcifications and soft plaques similar to how they have improved the accuracy of mammography in detecting breast cancers. Predictive algorithms and simulation software could also help predict the course of medical events and help develop a strategy for medical management or intervention. Finally, reimbursement barriers have to be overcome, by way of clinical data, to make this procedure more clinician- and prescription-friendly.
In 2010, more than 10 million Americans will experience chest pain.1,2 Of this population, about 950,000 will die from CAD—and of that number, 335,000 will die from heart attacks (also referred to as myocardial infarction (MI)) without being hospitalized.3,4 The estimated direct and indirect costs of treating patients with coronary heart disease is $177 billion in 2010.2
|
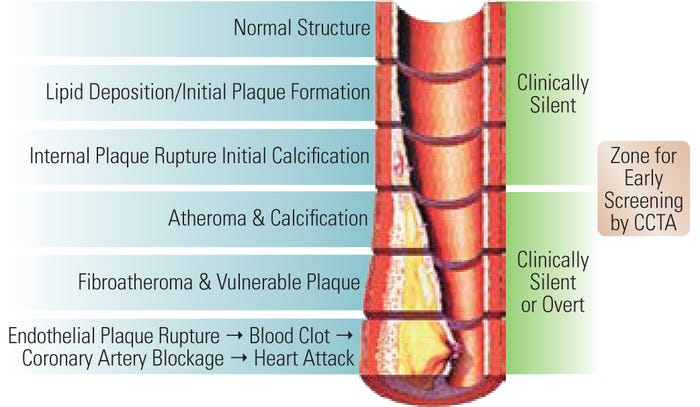
Figure 1. The progression of plaque in CAD. |
CAD is a condition in which there is an obstruction to the coronary blood vessel flow into the pumping heart muscle due to the formation of plaques. Plaques (fatty deposits within the walls of the coronary) are either vulnerable (soft) or nonvulnerable. The vulnerable plaques can be ripped during unaccustomed exertion (e.g., vigorous exercise without training), leading to platelet activation and blood clot formation. These factors increase the likelihood of obstruction, which can lead to a heart attack (see Figure 1).
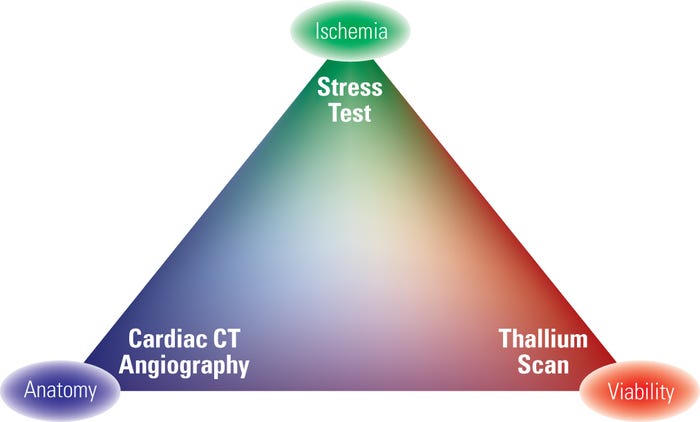
When investigating a patient with CAD, cardiologists need to know the anatomy of the arteries and blockage, the ischemia caused by the blockage, and the state of viability of the heart tissue (see Figure 2). Cardiologists use several tests to discover these traits: stress test electrocardiogram (ECG), thallium scan or perfusion studies, invasive catheter coronary angiography, coronary CT angiography (CCTA), and magnetic resonance (MR) angiography.5 This article focuses on CCTA.
CCTA is a noninvasive procedure performed by injecting a radiopaque dye into the patient and capturing the images of the heart from different angles using a CT scanner. This method provides anatomical information about the coronary arteries including the presence of blockages, plaques, and calcifications. Calcification is the deposit of calcium within the plaques inside the walls of coronary arteries and denotes advanced CAD. As per literature, calcium scoring, i.e., the measurement of total calcification in the coronary vessels, has a direct relationship with the longevity of the patient.6 A CT scan of the heart without a radiopaque dye can be used to determine the calcium score.
|
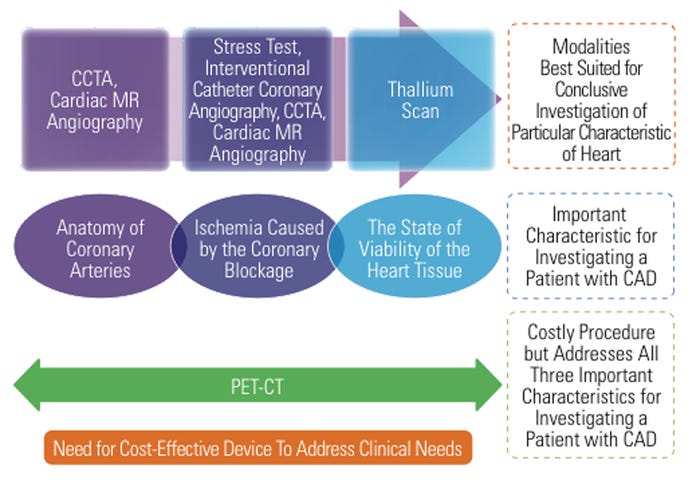
Figure 2. When investigating a patient with CAD, the cardiologist would like to know three important characteristics of the heart: the anatomy of coronary arteries and blockage, the ischemia caused by the coronary blockage, and the state of viability of the heart tissue. |
The recent integration of positron emission tomography (PET) and CT, although very expensive, meets the dream objective—an imaging technique that provides information about the anatomy, ischemia, and viability, in a single test. However, screening a large population with this type of expensive imaging is not feasible.7 To be effective in detecting undiagnosed CAD, the screening tool should not only have a high degree of reliability, high yield, and good validity, but it should also be cost-effective with a high degree of acceptance among physicians and patients.8
The authors designed a questionnaire and interviewed several interventional cardiologists across the United States to determine the feasibility of using CCTA as an early tool for the detection of CAD. Based on interview responses, CCTA is mainly useful in the following settings.
Emergency Settings. In the emergency room (ER), CCTA can quickly perform a “triple rule out” among MI or unstable angina, aortic dissection, and pulmonary embolism—all of which have acute chest pain as a primary symptom. CCTA is a simple procedure that can be performed in the ER as opposed to a nuclear stress test, MR angiography, or ECG stress test, primarily due to time constraints in the ER setting and the fact that a patient with acute chest pain may not be in a position to undergo some of these tests. Because more than 50% of ER visitors in the United States come in with chest pain, CCTA has clear applicability in the ER setting.9
Coronary Anomaly. CCTA is a niche diagnostic tool in cases in which interventional coronary catheterization cannot detect coronary artery anomalies (anatomical arterial abnormality).
High-Risk Patients with Abnormal Stress Test. Some high-risk patients with abnormal stress test results may not be able to undergo a coronary artery bypass graft, and CCTA is a good tool to help identify coronary artery plaques.
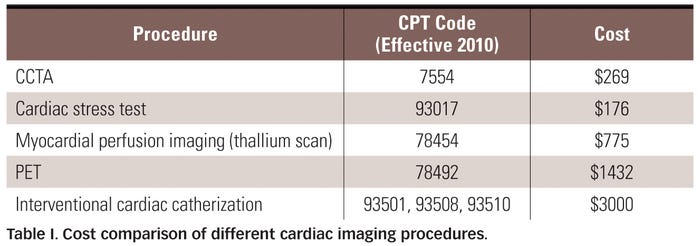
Symptomatic Patients with Stable Angina. CCTA is a noninvasive screening tool that can locate and measure coronary plaque. It is relatively cost-effective when compared with other cardiac imaging techniques (see Table I).
Asymptomatic Patients. CCTA can help in risk stratification and help manage patients to prevent major consequences of CAD. It is useful for patients who have no coronary symptoms but are at high risk of CAD due to a strong family history or other risk factors.
CCTA is a user-friendly outpatient procedure that can be conducted in about 30 minutes, and it is relatively cost-effective compared with other procedures.10 Although CCTA is not propagated as a standard screening tool for CAD in the United States, the negative predictive value of this procedure has made it a popular addition in routine physicals of corporate executives in some South Asian countries.
Economic dynamics and American Hospital Association (AHA) guidelines play an important role in limiting the wide use of CCTA for screening purposes. Most insurance companies in the United States do not reimburse for this procedure except for those indications currently listed in the AHA guidelines, such as for the detection of coronary anomalies. If the indications are further expanded in the guidelines to include screening for early detection of CAD and preventive management of impending MI, then CCTA may reduce heart attack deaths by bringing this asymptomatic population under preventive care. At present, health-conscious asymptomatic patients may have to pay out of their own pocket to take this test.
In addition, many interventional cardiologists interviewed said that cardiologists have a vested interest in not selecting CCTA because
They lose control of the patients as the case gets transferred to the imaging facility and to the radiologist.
If a large blockage is seen on a CCTA, they still have to proceed with therapeutic interventional catheterization anyway.
The reimbursement for interventional cardiac catheterization is far more than CCTA for the physician (see Table I).
The setup cost for CT scanners is high, unlike gamma cameras in thallium studies, and CCTAs' reimbursement coverage is relatively low in the United States.
One of the operational limitations for CCTA’s acceptance as a screening tool for CAD is the injection of a contrast agent and its nephrotoxic side effects. Additionally, the radiation dosage for a 64-slice scanner is anywhere from 4 to 16.3 mSv (millisievert) depending on gender and the physician performing it. According to FDA, “For a person without symptoms, CT screening is unlikely to discover serious disease, and the potential harm to the individual may be greater than the presumed benefit.”11 However, the response from some of the cardiologist interviewees was that the radiation effects caused by interventional coronary catheterization under fluoroscopy (the current gold standard for CAD diagnosis) is much higher than the radiation dosage delivered by CCTA. For symptomatic patients, radiation is not a problem; for asymptomatic patients, however, it is a concern because there could be false positives with CCTA, where the blockages might never progress to a symptomatic stage.
Interviewed cardiologists said that calcium scoring, i.e., plain CT heart scans without the injection of radiopaque dye to evaluate the calcium deposits in the coronary arteries, could be recommended every 10 years after age 40. This method could be alternated with a stress test every (other) five years. At present, CCTA is not considered a standard of care for detecting CAD by U.S. regulatory and reimbursing bodies, whereas stress tests, thallium scans, and ECGs are.
|
Figure 3. Opportunity area for a new or modified device as a screening tool for cost-effective and early detection of CAD. |
Despite the epidemic proportion of CAD, there is really no effective screening tool in place today to pinpoint coronary artery blockage as represented in Figure 3. CCTA can provide the objective evidence to bring a larger asymptomatic population with undetected CAD under medical management—to stabilize soft plaques and advocate lifestyle changes that delay the progression of the disease and the occurrence of heart attacks.
The Role of OEMs
There have been rapid advances with CT technology with the advent of multislice scanners. These high-resolution and high-speed systems obtain excellent images of the coronary arteries. With prospective ECG gating (heart being imaged while an ECG trace is recorded), the effective dosage of radiation could be reduced from 10–15 mSv to as little as 1.2 mSv. Currently, 64-slice scanners are widely available; however, 128-slice scanners have entered the market and are very good at identifying soft vulnerable plaques while keeping the artifacts low.
The software used in CCTA can be further improved to make it more intuitive, user-friendly, and especially to improve synchronization with regards to the ECG and diastolic heart images. To reduce the radiation exposure to the patient, there is an urgent need for the software to be able to self-check and measure the radiation exposure. The software should be able to create an alarm or shut the system down if the levels reach inappropriate ranges. This feature should be incorporated into the design of the CT system itself. Manufacturers can help by providing more outreach and educational training for technicians.
For CCTA to emerge as a viable screening procedure for the early detection of CAD, device manufacturers need to overcome certain barriers, including the lack of clinical evidence of efficacy or accuracy of predicting CAD. Clinical evidence–based amendments to AHA guidelines would eventually lead to improved reimbursement coverage from insurance companies. Finally, a drop in the setup cost of CT systems thanks to improved reimbursement coverage would facilitate greater acceptance by the medical fraternity.
Conclusion
There is an overwhelming need for a noninvasive, economical tool that can safely screen for significant coronary artery stenosis. CCTA, due to its low cost (almost 10 times less expensive than invasive catheterization) and high negative predictive value, is uniquely suited to address this need. The incorporation of new pattern recognition and predictive software tools into current high-resolution, high-speed CT systems might help increase the sensitivity of CCTA, allowing the method to be useful for ruling out soft plaques, a harbinger for impending heart attacks. Also, more clinical data are needed to convince the reimbursement bodies to expand the reimbursability of CCTA as a screening procedure.
References
1. S Boyles, “Cardiac Catheterizations: Too Many Performed?” Heart Disease Health Center, WebMD, March 2010; available from Internet: www.webmd.com/heart-disease/news/20100310/cardiac-catherizations-too-many-performed?src=RSS_PUBLIC.
2. “Heart Disease and Stroke Statistics—2009 Update, A Report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee,” Circulation 119, no. 3; available from Internet: http://circ.ahajournals.org/content/vol119/issue3/.
3. G Thorgeirsson, G Thorgeirsson, H Sigvaldason, and J Witteman, “Risk Factors for Out-of-Hospital Cardiac Arrest: The Reykjavik Study,” European Heart Journal 26, no. 15 (2005): 1499–1505.
4. “Sudden Deaths from Cardiac Arrest—Statistics, American Heart Association”; available from Internet: www.steeltonfire.com/ems/cardiacarrest.pdf.
5. MJ Shirani, “Advanced Cardiovascular Imaging: The American Experience,” Current Cardiovascular Imaging Reports 1, no. 1 (2008): 2–3.
6. P Greenland et al., “ACCF/AHA 2007 Clinical Expert Consensus Document on Coronary Artery Calcium Scoring By Computed Tomography in Global Cardiovascular Risk Assessment and in Evaluation of Patients With Chest Pain,” Journal of the American College of Cardiology 49, no. 3 (2007): 378–402.
7. M Vasken Dilsizian, “Keeping Current with the Latest Advances in Cardiovascular Imaging,” Current Cardiovascular Imaging Reports 1, no. 1 (2008): 1.
8. JMG Wilson and G Jungner, “Principles and Practice of Screening for Disease,” Public Health Papers No. 34, WHO 1968; available from Internet (pdf): http://whqlibdoc.who.int/php/WHO_PHP_34.pdf.
9. WE Cayley Jr., “Diagnosing the Cause of Chest Pain,” American Family Physician 72, no. 10 (2005): 2012–2021.
10. MJ Budoff et al., “Cost-Effectiveness of Multidetector Computed Tomography Compared with Myocardial Perfusion Imaging as Gatekeeper to Invasive Coronary Angiography in Asymptomatic Firefighters with Positive Treadmill Tests,” Journal of Cardiovascular Computed Tomography 3, no. 5 (2009): 323–330.
11. “FDA Unveils Initiative to Reduce Unnecessary Radiation Exposure from Medical Imaging,” FDA News Release; available from Internet: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm200085.htm.
Sudhi Gautam heads the Medical Solutions Group at Patni Americas Inc. (Milpitas, CA). Arathi Asthi is an intern at the company.
About the Author(s)
You May Also Like



.png?width=300&auto=webp&quality=80&disable=upscale)