Design & Engineering
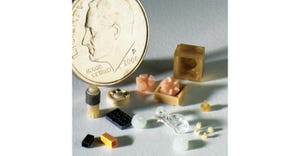
Widex SmartRIC (receiver-in-canal) hearing aid with portable charging case.
Design & Engineering
Behind the Design: Form Follows Function in New L-Shaped Widex Hearing AidBehind the Design: Form Follows Function in New L-Shaped Widex Hearing Aid
A Widex product designer shares insights behind the design of the company's newest hearing aid.
Sign up for the QMED & MD+DI Daily newsletter.





.png?width=700&auto=webp&quality=80&disable=upscale)




.png?width=300&auto=webp&quality=80&disable=upscale)


![Featured Image] 230916SF73.jpg Featured Image] 230916SF73.jpg](https://eu-images.contentstack.com/v3/assets/blt14ac89070d5e4751/blt381af30a9066bd0b/655b99d3323a8f040a9ee156/Featured_Image_230916SF73.jpg?width=300&auto=webp&quality=80&disable=upscale)