June 3, 2014
For information on sterility assurance levels (SALs), see "How Can You Ensure that Your Device Is Sterile?" |
When sterilizing medical devices, sterilization personnel rely on bioburden counts as part of determining and maintaining the sterilization process. In the following Q&A, Martell Winters, senior scientist at Nelson Laboratories (Salt Lake City), discusses less-than values in bioburden testing and explains how bioburden alert and action levels are an important part of ensuring the sterility of medical devices. At MD&M East on June 10, he will return to this theme in a presentation titled "Setting Alert and Action Levels for Product and Environmental Bioburden Counts."
MPMN: Please explain bioburden and why collecting bioburden data is important.
Winters: When validating medial devices, there are two main types of sterilization: the overkill and the bioburden-based approaches. Most sterilization methods (for example, ethylene oxide and steam) use the overkill approach, which assumes a worst-case bioburden of 1 million of the hardest-to-kill microorganisms, known as spore forming microorganisms. Since overkill cycles assume this worst-case count, the bioburden on the product is less critical unless the counts are extremely high--for example, unless they approach 1 million. However, this is very seldom the case. Products usually leave the manufacturing environment with bioburden counts in the hundreds or less unless the device is very large and complex, in which case the counts can be higher.
|
Bioburden analyst filters solution through a membrane filter. |
The more common overkill processes are ethylene oxide (often called EtO) and steam (also known as autoclaving). Although they can be high, bioburden levels are still important from a trending standpoint because they enable the OEM to understand how well the manufacturing environment and the assembly personnel are controlled. But it is less critical from a sterilization standpoint because of the huge overkill factor built into the cycles.
With radiation sterilization, spore forming microorganisms are not the most resistant types of microorganisms. Consequently, the overkill method doesn't work for radiation sterilization. Thus, radiation sterilization requires the use of the bioburden approach, in which the bioburden count on the product determines what the sterilization dose should be.
MPMN: Could you go into the role of less-than values?
Winters: Before discussing less-than values, the test method must first be explained. When performing a bioburden test to determine the number of microorganisms on a product, the technician cuts or disassembles the device to expose all of the surfaces, both external as well as internal. The pieces are then put in a bottle, to which a sterile solution is added. The bottle is shaken in order to remove the microorganisms from the device and to suspend them in the solution. Then, the solution is filtered to trap the microorganisms, after which the filter is placed on an agar plate or petri dish. This procedure allows the microorganisms to grow into visible colonies. A colony begins with one microorganism or a clump of microorganisms, which then grow into a colony that is visible to the naked eye. This colony count on a plate roughly equates to the number of microorganisms on the product.
|
|
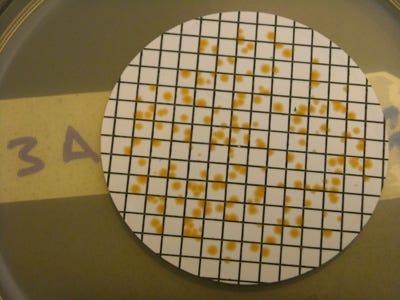
Bioburden agar plates contain colonies of microorganisms on a membrane filter. |
In the filtration phase of this testing, most of the solution is sometimes filtered. Let's say that 200 ml of solution are needed to cover the device while it's being shaken. In that case, 100 ml of the solution might be filtered, and then the filter is placed on an agar plate. In this example, the colony count grown on the filter after incubation is then multiplied by a factor of two to get a total count because only half of the solution was filtered. If the device is clean--meaning that no microorganisms have been detected on the filter--it still cannot be said that there are zero counts because not all of the solution was filtered. There could have been one or two microorganisms in the other half of the solution.
Regardless of the multiplication factor used to represent the entire product, it is not acceptable to report zero microorganisms, even if no microorganisms are detected on the filter. A value of <2 is reported because of the limit of detection (LOD) or the limited sensitivity of the test. Such values are called less-than values. Less-than values are not much of a problem if they are very low--for example, <1 or <2. But because of the nature of the product or other factors, sometimes a very small portion of the solution ends up getting tested--perhaps only 1/10. In such cases there is a multiplication factor of 10, and if there is no microbial growth on the filter, it is reported as <10 CFU (colony-forming unit).
Thus, less-than values become more significant when a smaller percentage of the extraction solution is filtered. Less-than values become a greater issue when dealing with combination products, biologics, or tissues, where low radiation doses might be required. In other words, the sensitivity of the test must be very good. For example, if the bioburden result is <10, the lower radiation sterilization doses of 15 or 17.5 kGy are not an option.
MPMN: Please go into setting alert and action levels for bioburden counts. How is this done and what does it accomplish?
Winters: Alert and action levels are sometimes set in a very arbitrary manner. Sometimes companies select a number out of the blue, or sometimes they select a value obtained from previous data and use it. One goal of some experts in the medical device industry is to help companies be more selective and scientific in determining alert and action levels. A couple of factors should be considered in determining these levels.
The first factor is the type of sterilization method. Returning to the overkill method, in which the sterilization process assumes a high number of spore forming microorganisms, one should allow a higher bioburden count on the product because the bioburden on the product must become very high before it potentially begins to impact the sterility assurance level (SAL) of the sterilization process. But with radiation sterilization, in which the radiation dose is very closely tied to the bioburden count, stricter bioburden controls are preferable. Thus, the first item to consider in determining alert and action levels is which sterilization process will be used in a given instance. This will help sterilization personnel to understand whether or not they wish to allow a more flexible bioburden count on the product.
The second factor is to review historical bioburden data to determine what types of bioburden ranges have been obtained in the past. Unfortunately, people will sometimes set alert and action levels without relying on historical bioburden data. Again, they simply pick a number. But the acceptable bioburden counts for a particular device should normally be based on actually obtained bioburden data. Although bioburden counts don't directly affect such sterilization methods as EtO, it is still necessary to demonstrate control over the product's bioburden levels, the manufacturing environment, and the personnel. And monitoring bioburden counts is one of the best ways to accomplish this objective. Even when setting alert and action levels to products that will undergo EtO sterilization, it is not wise to set an alert and action level at very high bioburden counts, such as 1 million. It is best that it be at levels that will enable a company to demonstrate good control over the product and the manufacturing process.
Usually when establishing bioburden levels, two separate values are appropriate. The alert level represents a bioburden count that might have shifted outside of the norm. Thus, if the data hit an alert-level bioburden count, the sterilization process is likely not affected, but something might be happening to cause the bioburden to change. In most cases, an alert level does not require any actions. It simply indicates that the sterilization personnel should be more aware of the situation. It might be appropriate to investigate why the changes are taking place--for example, have materials from a new supplier been used in the product that might have caused the bioburden to increase?
The action level is often set at a level where sterilization personnel fear that bioburden has increased to such a level that it might begin to impact the sterilization process. In other words, the sterilization process might not provide the 10-6 SAL target values stipulated in the regulatory files. The action level should be higher than the alert level and should allow for flexibility. The action level should not be set so low that it is triggered frequently. When the action level is triggered, this indicates that something has definitely changed in the manufacturing process and that some type of investigation is required. Common aspects of the investigation include a review of the suppliers and manufacturing process and additional testing to determine if the change is consistent or a single event.
Bob Michaels is senior technical editor at UBM Canon.
About the Author(s)
You May Also Like