Originally Published MDDI June 2006 WASHINGTON WRAP-UP Although the CDRH director praises industry’s technological advances, recalls and adverse event reports are still on the rise. James G. Dickinson
June 1, 2006
WASHINGTON WRAP-UP
|
Medical device safety is looming as a major concern. Recalls have risen 20% over the last three years, despite 10 years of experience with the QSR. In addition, reported adverse events involving medical devices have risen 50% over a six-year period.
Daniel Schultz sought to balance these troubling trends with a buoyant view of industry's technological advances. Speaking at the RAPS Horizons 2006 Conference in San Diego at the end of March, the CDRH director admitted that the adverse reactions trend might not tell the whole story. He noted that such incidents are “largely underreported.”
Saying he'd “had no idea how difficult” managing the adverse events issue would be, Schultz indicated he is not alarmed by the rising recalls. “I don't think it should come as much of a surprise,” he said. “We're seeing more devices that are doing more-complicated things with respect to people's health. So when we start seeing more adverse events and recalls, I think to some extent it is a consequence of our own success.”
But, he added, FDA needs to figure out how to manage the trend. The agency must ensure that there is continued public confidence that medical devices are helping rather than hurting people.
|
Although he says managing adverse event issues is very difficult, Schultz is not alarmed by the rising recall rate. |
Schultz cited Section 104 of the Medical Device User Fee and Modernization Act of 2002 (MDUFMA). It requires FDA to submit a postmarket safety report to Congress by next January. The report will be used to help justify renewal of the user-fee legislation.
Schultz said it's important to keep device positives in mind. “When we hear about postmarket issues,” he said, “we only hear about the risks. I think it's really important that we be able to transmit this information—not just in terms of isolated risk, but also putting it in context and being able to talk about ongoing risk-benefit issues. Whether they be positive, or less positive, or more positive, we need to be able to explain things in a way that people can understand.”
Schultz acknowledged unexpected challenges in tackling postmarket issues. “Devices are becoming smaller and more complex,” he said. “There's less margin for error, and implanted devices are being used for longer periods of time and in younger populations. Our resources in terms of the field have been shrinking over the last few years, and our ability to go out and inspect to the extent and degree that we'd like is limited. We certainly have challenges with regard to our ability to communicate this [risk-benefit] information as we would like to,” he continued.
“We've identified specific challenges with regard to adverse event reporting,” Schultz said. “We know that adverse events are largely underreported. We receive a number of reports with inaccurate information about how the device was used and what may have caused the problem.”
Sidebar: Critical Path Collaborations |
He also noted that the center often has trouble identifying the specific devices involved. Healthcare professionals generally do not document device use in patient records, many devices lack unique identifiers, and manufacturers continually produce modified versions of their products. So, he said, “sometimes it's really difficult to figure out what model was actually involved. Implants are not returned for analysis. Devices are often used off-label.”
And, he explained, FDA is seeing a shift from traditional hospital-based medical care to home-based medical care. As home care becomes more prevalent, getting the reports done and understanding what may be causing problems may become even harder.
Schultz emphasized that a unique-identifier system is urgently needed for medical devices. However, he recognizes that there are technological barriers. Also needed, he said, is an electronic reporting system.
In response to a question about why recalls continue to increase 10 years after the introduction of the QSR and while risk management issues are already so prevalent, Schultz seemed caught off balance. After a long pause, he said it would be “simplistic” to only have a goal of reducing recalls.
Many recalls continue to cite recurring, similar problems “over and over again,” he admitted. Perhaps better QSR training is needed, he wondered out loud. Complaint handling is a constant problem, for example, as are corrective and preventive action programs. “We have not done a very good job in explaining what needs to be done,” he noted.
Schultz's speech began with a sharp focus on more-upbeat matters. He pointed to the now rapidly growing inclusion of medical devices within FDA's much-trumpeted and drug-dominated Critical Path Initiative. Schultz explained that divisions between drugs, biologics, and devices are blurring. “This sort of distinction may become moot within the not-too-distant future,” he said. “Certain things are common to the development of all these different product lines.”
Infusion Pumps Lead the Pack in Recalls
|
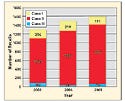
Figure 1. Medical device recalls have risen over the last three years. Source: CDRH. |
The number of medical devices recalled has increased nearly 20% in three years. Recalls are up from 1300 in FY 2003 to 1490 in FY 2004 and 1598 in FY 2005, according to Timothy Ulatowski, the CDRH compliance director. Ulatowski presented these data at the Medical Device Congress at Harvard University in March (see Figure 1).
Ulatowski said 25 infusion pumps were recalled in FY 2005, putting that device in the top recall spot for the year. Other top spots included an intravascular administration set, nuclear MRI system, heart valve allograft, implantable defibrillator, automatic external defibrillator, and continuous ventilator. Rounding out the top 10 were an automated differential cell counter, an introducer catheter, and an intravascular catheter.
Recall problems, he said, include determining whether a recall should be Class I and a lack of timely, accurate, and comprehensive communication. Also problematic are QSR deficiencies such as mandatory Section 806 reports, handling of complaints, trending, risk assessment, and corrective and preventive actions. Many companies also struggle with implementing a recall strategy.
|
Figure 2. Corrective and preventive action (CAPA) was the area cited most often on FDA-483s during FY 2005. Other types of observations also posted large numbers. Source: FDA. |
The leading observation from the FDA-483s during FY 2005 inspections was corrective and preventive actions, with 219 citations (see Figure 2).
Legal and administrative actions have been slowing, said Ulatowski. FDA issued 182 warning letters in FY 2005, down from 219 the previous year and 205 in FY 2003. Injunctions, seizures, monetary civil penalties, and civil contempt citations have remained flat over the three years.
U.S. May Crack Down on Off-Label Claims
In what may signal a new wave of government scrutiny, the U.S. Attorney's Office in Philadelphia has issued a grand jury subpoena to a device firm. Pennsylvania-based Synthes Inc. has been subpoenaed over alleged off-label promotion practices. Until recently, off-label prosecutorial cases have been limited to drug makers. But prosecutors have been warning that federal investigations are likely to spill over into the device arena.
High-profile government prosecutions against drug companies over their marketing practices have been on the rise. Several months ago, Jnatel Simmons noted that “there is no reason the medical device industry would be immune to prosecution.” In fact, she said, they're the likely next target. Simmons is senior counsel at the HHS Office of Counsel to the Inspector General (OIG). She spoke at the RAPS annual meeting in Baltimore last October.
Simmons said most government actions against medical device firms originate as qui tam actions or whistleblower lawsuits under the False Claims Act. The act prohibits falsified claims for payment from being submitted to the government. These claims often involve allegations of kickbacks being offered in exchange for business that is reimbursable by a federal healthcare program, she added.
The latest subpoena demands that Synthes supply information on alleged off-label promotion practices for its Norian XR bone void filler and related products. The Department of Justice appears to be investigating the promotion, sale, and reimbursement of Norian XR, according to the company.
A 510(k) was cleared in December 2002 for use of Norian XR in certain bony voids or defects that are not intrinsic to the stability of the bony structure. The product was removed from the market in November 2004, after an FDA inspection and subsequent warning letter. In it, the agency charged that the company was marketing Norian XR for new intended uses without FDA approval. These alleged new uses included vertebroplasty and kyphoplasty.
|
Laemmle-Weidenfeld predicts that future false-claims cases will stem from state Medicaid program problems. |
Cases filed under the False Claims Act are being brought primarily by two of the largest offices of the U.S. Attorney in the country—Boston and Philadelphia—according to Patton Boggs partner Laura Laemmle-Weidenfeld. She predicted that companies will see additional prosecutions coming from these offices “because the prosecutors know what they are doing, they know how to run these cases, and at this point they know the relators bar very well.”
Additionally, as state Medicaid programs continue to struggle, she said, it's likely that some false-claims investigations will originate with these programs, which may also take a much more active role in federal probes.
FDA Takes Steps on Postmarket Studies
CDRH has taken a number of “action steps” to satisfy critics who had earlier cited it for failure to follow up on postmarket studies, said CDRH epidemiology branch chief Danica Marinac-Dabic. Such studies are required as conditions of approval (CoA) for new medical devices. Speaking at FDLI's annual conference in Washington, DC, in April, Marinac-Dabic said there now exists a “culture of collaboration” within the center that is strongly focused on postmarket safety.
She said the center's epidemiology staff is now involved in premarket approval (PMA) reviews to help design better postapproval studies. A tracking system has also been developed to better enable postmarket staff to follow up on CoA studies to ensure that they are satisfactorily performed. She said that the agency has recently issued a guidance to industry specifying how CoA follow-up reports should be submitted.
Marinac-Dabic says a key aspect of CDRH's new emphasis on postmarket safety is its willingness to work with outside entities to improve its program. “For example,” she said, “CDRH is working with AdvaMed and the Heart Rhythm Society to improve the format of the agency's Product Performance Reports, the PMA annual report, and standardized ‘Dear Doctor' letters.” She said that the agency is also working with AdvaMed to make overall improvements to the postapproval studies program. CDRH's ability to take enforcement actions is also being strengthened internally by improving the coordination, consistency, quality, and timeliness of inspections that lead to enforcement actions.
Sidebar: AdvaMed Working Groups |
Joseph Levitt, a 25-year FDA veteran and former CDRH associate director for regulation and policy who now works for Hogan & Hartson, has traced the legislative authorities available to CDRH to enforce postmarket safety programs applicable to medical devices. He began with those found in the Medical Device Amendments of 1976. This initial legislation defined adulteration and misbranding as applied to devices and also required reporting of adverse events and specified registration, listing, and inspections for device manufacturers. It also imposed controls for imported devices. Additional postmarket authorities, passed in 1990, the Safe Medical Devices Act, included requirements governing mandatory recalls, authorized temporary suspension of PMAs, and imposed requirements for tracking in-use devices.
“Device authorities are now far more extensive than for prescription drugs,” Levitt said. “FDA and CDRH should focus on existing authorities to develop strategies for meeting safety challenges to devices rather than to seek new legislation.” He said device makers and end-users should work with CDRH to find solutions to any unresolved regulatory problems.
AdvaMed executive vice president for technology and regulatory affairs Janet Trunzo agreed with Levitt. She said CDRH possesses enough authority to enforce postmarket safety programs for medical devices. She also repeated his assertion that CDRH should concentrate on refining and improving existing systems.
AbTox Executives Convicted
A federal jury in Chicago has convicted AbTox president Ross Caputo and regulatory affairs director Robert Riley for marketing faulty sterilization equipment to hospitals. They had been indicted on mail and wire fraud charges arising from selling sterilizers that were not approved by FDA. The sterilizers deposited toxic copper and zinc salts on devices. AbTox sold 168 sterilizers to hospitals around the country from 1994 to 1998 for $18 million. The faulty equipment left 18 people blind in one eye. Sentencing is set for July 12; both men face up to 12 years in prison.
Blackstone Recalls Fixation Implant
Blackstone Medical has issued a Class 1 recall for its Icon Modular Fixation System because of the potential for components to fail after implantation. The Icon system is composed of components that surgeons must assemble and construct. The components include screws, connectors, and rods that, when assembled, are implanted in and near a patient's spine. The system is intended to immobilize and stabilize spinal segments at the site of spine surgery. “The potential for injury due to failure of the implant will depend on the specific condition being treated and the degree of postoperative healing,” according to a company notice.
Copyright ©2006 Medical Device & Diagnostic Industry
About the Author(s)
You May Also Like