April 4, 2014
Whether it involves utilizing a natural material such as silk or altering material surfaces at an extremely tiny level to make them more biocompatible, recent innovations are promising to allow for better-performing orthopedic implants.
|
Surgical plates and screws made from pure silk protein not only offer improved bone remodeling, but also can also be absorbed by the body over time--eliminating the need to cut someone open again to retrieve them, according to David Kaplan, PhD, Tufts University's chair of biomedical engineering. |
One recent example involves surgical plates and screws made from pure silk protein. They not only offer improved bone remodeling, but also can also be absorbed by the body over time, according to a research team from Tufts University School of Engineering and Beth Israel Deaconess Medical Center.
Peoria, AZ-based Nasseo meanwhile won FDA clearance last fall for its TiArray Dental Implant System that uses a special titanium dioxide nanotube surface to make its titanium screws more bone growth-friendly, hopefully creating a bond between the implant and bone quickly enough to prevent inflammation from developing.
Some of the advances have been aided by better electron microscopes and imaging technologies that can allow researchers to really see what they are creating at a nano-sized level.
"Twenty years ago, we didn't have the advanced imaging technology so you can see what you're modifying at that level," says Nasseo CEO Garrett Cale Smith, PhD, co-inventor of the nanotubes technology with material sciences professor Sungho Jin, PhD, at the University of California, San Diego.
The advances are also simply the fruits of years of tinkering and sweated out research. Smith estimates more than 50 published studies related to Nasseo's technology. David Kaplan, PhD, Tufts' chair of biomedical engineering, has spent 25 years studying silk, grasping the fundaments, and perfecting how to purify it so that its proteins could be used in implants.
"My whole career has been working on silk, start to finish," Kaplan said.
There are plenty of hurdles still to overcome before such advances become commonplace in the orthopedic space.
"These two technologies are both interesting from the orthopedic device maker's point of view, although both appear to be relatively early in the development pathway," says David Armbruster, global program manager at Johnson & Johnson's DePuy Synthes Biomaterials. (Armbruster made it clear that his opinions were his own, not DePuy's.)
The potential success of such technologies, though, is serious business because orthopedic implant infections can be devastating. Bacteria can produce antibiotic-resistant "biofilms" around the implants.
Mayo Clinic estimates that the total number of U.S. hip arthroplasty and total knee arthroplasty implantations alone will increase from approximately 600,000 to 4,000,000 by 2030 as the active but aging baby boom generation replaces is worn out joints. Assuming a 1% to 5% risk of infection from all prosthetic joints, Mayo expects the incidence of such infections to skyrocket at a similar pace.
The work by people such as Kaplan, Smith, and Jin could help stem the tide if successful.
A Silk Road to Ortho Innovation
Kaplan himself likes to point out that silk is actually a pretty old-school medical material. Get stitches at an emergency room, and the sutures are still likely made of silk, just as they were a hundred years ago.
"Nobody figured out that you could actually clean that material up and use it for all kinds of medical devices, despite it being around for hundreds of thousands of years," Kaplan said.
The major hurdle when it comes to using it for implants has been the impurities--contaminating, glue-like proteins made by the worm.
"If you put a textile silk in the human body, you would have huge problems because it is not very pure. ... We don't need those [glue-like proteins]. When they are associated with the core protein, they cause biological problems," Kaplan said.
Kaplan spent about a dozen years figuring out how to remove the impurities.
"You start where the textile makers leave off, and then you refine for ultra-purification. ... The core material is what you want to purify. It's all just process control. It's time, temperature, concentration, those kinds of variables," Kaplan said.
Once the proteins were purified out, the next step was figuring out how to coax them to fold in order to produce more solid materials. (Anyone who has had to continually iron a silk shirt knows that silk has no problem folding.)
Silk protein obtained from Bombyx mori (B. mori) silkworm cocoons had to be folded in complex ways to give it exceptional properties when it came to strength and versatility. (Kaplan says he and his colleagues have produced silk implants reaching the low end of the range of strength seen in bone.)
The next step was to try out 28 silk-based screws in six laboratory rats, with assessments conducted at four and eight weeks after implantation. None of the screws failed.
Surgical plates and screws made from pure silk protein not only offer improved bone remodeling, but also can also be absorbed by the body over time--eliminating the need to cut someone open again to retrieve them, according to Kaplan.
There's another advantage Kaplan sees in silk: Plates and screws made of silk could actually deliver antibiotics to prevent infection, pharmaceuticals to enhance bone regrowth and other therapeutics to support healing.
The research on silk-based orthopedic implants was published in March in the journal Nature Communications.
The silk-based screws might initially be used to treat the hundreds of thousands facial injuries that take place annually. But there is also potential to treat a variety of bone fractures with them, says Samuel Lin, MD, of the Division of Plastic and Reconstructive Surgery at Beth Israel Deaconess Medical Center and associate professor of surgery at Harvard Medical School. Lin co-authored the Nature Communications study with Kaplan.
Current bioabsorbable polymers used in orthopedic surgery have some limitations, including acidic degradation products and low strength relative to titanium, according to Armbruster.
"If mechanical implants such as plates and screws made from silk have improved strength they would be very interesting for more load-bearing applications. If implants made from silk proteins degrade in a more tissue-friendly way, they may be attractive for applications such as ACL interference screws, which release a large quantity of degradation products over time," Armbruster said.
Armbruster, though, cautions that key questions such as material cost, ease of processing, and in vivo safety must still be answered to determine if silk will be commercially viable.
Refresh your medical device industry knowledge at MD&M East, June 9-12, 2014 in New York City. |
Silk from caterpillars isn't the only naturally derived material that has been getting attention from medical device designers lately.
Last year, a group of U.S., Iraqi, and Spanish research reported that they had demonstrated proof of concept for a heart pulse sensor and current-driven actuator devices based on spider silk coated with functionalized carbon nanotubes.
The researchers--from Florida State University, University of Baghdad (Iraq), Institut de Ciencia de Materials de Barcelona (Spain), and Institucio Catalana de Recerca (Spain)--found the coated fibers are four times tougher than neat silk fiber, versatile and multi-functional, and exhibit polar, shapeable, conducting, flexible, strain- and humidity-sensitive properties, according to their paper in Nature Communications.
Meanwhile, Carnegie Mellon University's Chris Bettinger and Jay Whitacre found that cuttlefish ink provides just the right chemistry and nanostructure to power tiny, ingested electronic devices.
Nanotubes Driving Next-Gen Orthopedic Technology
Meanwhile, nanomaterial advances are set to greatly increase the performance of orthopedic implants.
Peoria, AZ-based Nasseo last fall won FDA clearance for its TiArray Dental Implant System that uses a special titanium dioxide nanotube surface to make its titanium screws more bone growth-friendly, hopefully creating a bond between the implant and bone quickly enough to prevent inflammation from developing.
|
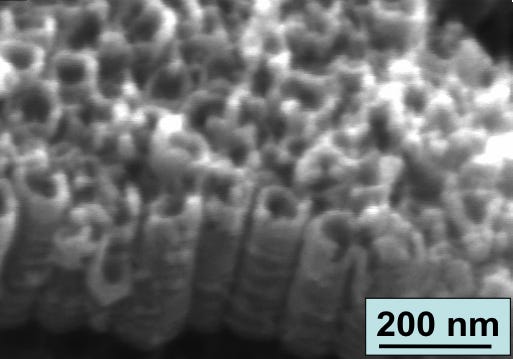
Micrographs from Nasseo show structures of the vertically aligned TiO2 nanotubes on titanium substrate. |
Nasseo is one of a number of innovators seeking to make orthopedic implants much more biologically compatible by altering surfaces at the nano level. Others include Columbia City, IN-based Nanovis, which has technology for nanopatterned surfaces on implant metals, polymers, ceramics, and ceramic composites. There's also the work of Thomas Webster, who directs the Nanomedicine Laboratory at Northeastern University.
Nasseo's nanotube surface is all about "essentially mimicking porous bone at the nano and molecular scale," according to Nasseo's co-founder and chief operating officer Kayvon Pourmirzaie.
"You want to see all these cascading impacts that occur for bone remodeling. ... Reducing inflammation is key," Pourmirzaie says.
The surface technology is licensed from the University of California, San Diego, where researchers led by the material sciences professor Jin spent more than eight years fine-tuning a secret sauce of chemical processes, anodizing and heating that altered the 5 nm titanium dioxide surface already naturally present on CP4 titanium.
"What you end up with are 300 nm nanotubes that are patterned and uniform across the surface," Pourmirzaie says. (Smith, the Nasseo CEO, was a co-inventor.)
Trials are starting at the Arizona School of Dentistry and Oral Health.
Orthopedics device makers for years have been making metal materials porous down to levels of a millionth of a meter. The technology Nasseo is using, however, is creating a porous surface at billionth of a meter levels.
Smith and Pourmirzaie see a wide variety of opportunities--including enhancing the porous metals already out there and coating plastic orthopedic parts, such as PEEK modulus for spinal implants, to make them more bone friendly.
It is also more soft tissue friendly. Biologics and drug delivery might also be enhanced with the nanotubes surface.
Armbruster agrees: "The surface porosity could in theory be an elegant method for drug delivery as well, allowing drug to be coated into rather than onto an implant surface, and eliminating the need for a carrier matrix. Whether this technology can be used to modify existing implants in a way that provides a clinical benefit will need to be demonstrated in future studies."
Chris Newmarker is senior editor of MPMN and Qmed. Follow him on Twitter at @newmarker.
About the Author(s)
You May Also Like