Medical Device & Diagnostic Industry MagazineMDDI Article IndexOriginally Published September 2000 Advances in balloon technology have opened up endless design possibilities, including both specialized and multifunctional devices.Mark A. Saab
September 1, 2000
Medical Device & Diagnostic Industry Magazine
MDDI Article Index
Originally Published September 2000
Mark A. Saab
Recent advances in the design and fabrication of high-pressure medical balloons have enhanced their performance capabilities and broadened their use into new applications in the device industry. Developed in the late 1970s, high-pressure balloons have traditionally been used in angioplasty, a procedure that opens a blood vessel clogged by a buildup of fatty plaque. The balloon, tightly wrapped around a catheter shaft to minimize its profile, is inserted through the skin and into the narrowed section of the vessel. Inflating the balloon—typically with saline or a radiopaque solution forced through a syringe—exerts high pressure, which compresses the plaque against the wall of the vessel and allows the blood to flow normally. For retraction, a vacuum is pulled through the balloon to collapse it. The procedure was developed as a less-invasive and less-costly alternative to coronary bypass, a complex surgical procedure that skirts the blockage by grafting a section of vein, usually taken from the leg, to locations above and below the afflicted area.

Angioplasty balloons come in a range of sizes, from coronary artery-sized versions to large-diameter models for peripheral vessels.
Today's high-pressure medical balloons—with thinner walls, higher strength, and smaller profiles—are well suited for use in a broad range of minimally invasive procedures. They can be produced in a variety of lengths, diameters, and shapes, including complex custom shapes for specific applications, and supplied with specialty coatings for added performance. Innovations in balloon design and technology have provided increased flexibility to product designers, making the development of new and improved devices possible. As a result, high-pressure balloons are being employed in a growing number of diagnostic and therapeutic procedures. Applications include the following:
Angioplasty catheters.
Other dilatation catheters.
Stent-delivery catheters.
Heat-transfer catheters.
Photodynamic therapy devices.
Laser balloon catheters.
Cryogenic catheters.
Drug-delivery devices.
Positioning catheters.
Arthrectomy catheters.
It should be noted that many of the applications and procedures discussed in this article are experimental and have not yet been cleared for commercial use by FDA.
BASIC BALLOON TYPES
Two basic types of balloons are used in the medical industry. This article is primarily concerned with the first type: high-pressure, nonelastic dilatation- or angioplasty-type balloons used to apply force. The second type comprises low-pressure, elastomeric balloons, typically made of latex or silicone, that are used primarily in fixation and occlusion.

For drug delivery applications, two discrete balloons or a dog bone–shaped balloon can be used to seal off the precise area that requires treatment, thus sparing healthy surrounding tissue.
The two types have few similarities. High-pressure balloons are molded to their inflated geometry from noncompliant or low-compliant materials that retain their designed size and shape even under high pressure. They are thin walled and exhibit high tensile strength, with relatively low elongation. Low-pressure balloons are typically dip molded in a tubular shape, and are then expanded to several times their original size during use. Thus, these balloons cannot be inflated to precise dimensions and cannot retain well-defined shapes, nor maintain high pressures.
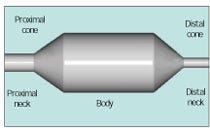
Figure 1. A standard balloon consists of a cylindrical body, two conical tapers, and two necks.
For angioplasty, balloons must have a controllable or repeatable size (diameter versus pressure) in order to ensure that they will not continue to expand and damage or rupture the artery after opening a blockage. Balloon compliance is the term used to describe the degree to which the diameter of a high-pressure balloon changes as a function of pressure. For example, a low-compliance, high-pressure balloon might expand only 5–10% when inflated to the rated pressure, whereas a high-compliance, high-pressure balloon might stretch 18–30%. Conversely, low-pressure elastomeric balloons—which are inflated by volume, not pressure—can stretch 100– 600%; when the pressure is released, they recover close to their original size and shape. Such balloons generally cannot be used to exert high pressure in medical applications.
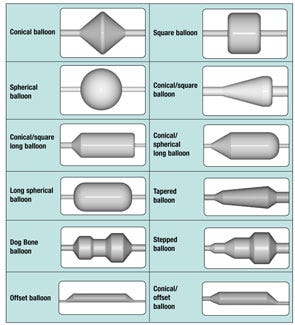
Figure 2. Examples of high-pressure balloon shapes. A specific shape may be demanded by the particularities of the anatomical site, ther requirements of the treatment process, or both. (The designs shown here can be formed in different diameters and lengths.)
HIGH-PRESSURE BALLOON MATERIALS
The first angioplasty balloons were fabricated from flexible polyvinyl chloride (PVC). They were relatively thick walled and designed for low pressure, compared with today's high-pressure balloons. Cross-linked polyethylene came into use in the early to mid-1980s, about the same time that polyethylene terephthalate (PET) was adopted for high-pressure balloons; to a large degree, these two materials replaced PVC. Nylon balloons were introduced in the late 1980s, and polyurethane balloons followed in the early 1990s. Nylon, though not as strong as PET or as compliant as polyethylene, was seen as a compromise because it is relatively strong and can be used in relatively thin designs. Currently, most high-pressure medical balloons are made from either PET or nylon. PET offers advantages in tensile strength and maximum pressure rating, whereas nylon is softer. Table I shows a comparison of various high-pressure balloon materials.
Rated pressures for angioplasty balloons are typically in the range of 2–20 atm (from 30 to nearly 300 psi), depending on the size. In general, the larger the diameter, the lower the rated pressure: as the diameter of a balloon increases, the stress in the balloon wall also increases when inflated to its nominal diameter. One major advantage of PET is its unusual ability to be molded into ultrathin walls from 5 to 50 mm (0.0002 to 0.002 in.) and very precise shapes, enabling PET balloons to have extremely low profiles.
High-pressure PET balloons can be produced with diameters from 0.5 to 50 mm or more, in any working length, with very thin walls. They can be custom designed with varying diameters along the length of the balloon, and with tapered ends from 1° to 90°. Other benefits include excellent heat-transfer characteristics and optical clarity, making PET balloons suitable for energy delivery via Nd:YAG and other lasers or ultrasound and microwave equipment.
Compared with PET versions, nylon high-pressure balloons require a thicker wall for a given burst pressure. This generally means that a nylon balloon will have a larger profile than a comparable PET balloon upon insertion into the body and when crossing a lesion. However, because nylon is softer, it is more easily refolded and is easier to withdraw into the guiding catheter or introducer sheath.
A wide variety of coatings can be added to the surface of a balloon to enhance or alter its properties to meet new requirements. Balloon coatings include formulations designed to modify lubricity (both hydrophilic and hydrophobic coatings), abrasion and puncture resistance, conductivity, thrombogenicity, drug release, and reflectivity, among other characteristics.
BALLOON MECHANICS
Virtually all high-pressure balloons are fabricated by first extruding a tube or preform, cross-linking the extrusion (if required), then reheating and stretch–blow molding the extrusion into the desired geometry. A standard dilatation balloon consists of a cylindrical body; two conical tapers; and two necks, proximal and distal (Figure 1).
The stresses in a standard balloon are represented by the following equations:
r = pd/2t, s1 = pd/4t
where p = pressure, d = diameter, t = thickness, sr = hoop or radial stress, and sl = axial or longitudinal stress. From the above equation, the calculated radial tensile strength (TS) of a balloon can be easily calculated as follows:
TS = pd/2t
where p = burst pressure, d = diameter (as made), and t = thickness (as made). Fortunately, the radial (or hoop) stress is twice the longitudinal stress; therefore, when a balloon fails, it normally splits along its length rather than circumferentially. This is preferable in a clinical sense, since radial or circumferential balloon failures can cause complications in medical procedures.
BALLOON ENDS AND SHAPES
High-pressure balloon ends are available in a variety of forms: conical sharp corner, conical radius corner, square end, spherical end, and offset neck, with other more-complex forms also possible. The choice of an end form depends on the requirements of the end-use procedure.

Figure 3. Balloons for carpal tunnel dilatation: the balloon as formed (top); the inflated balloon in its assembled state (middle); the deflated balloon profile (bottom).
The shape of the balloon body can also vary from the standard shape shown in Figure 1. It can be sectioned into different diameters and lengths (e.g., dog bone–shaped and stepped balloons) or fashioned and shaped into a conical, square, or spherical shape (or a combination of these). If required by the application, different ends can also be used on the same balloon. Some examples of high-pressure balloon shapes are shown in Figure 2.

Figure 4. A coronary stent, at minimum diameter, is crimped over a balloon and ready to be inserted into an artery.

Figure 5. The coronary stent expanded by the balloon. The balloon presses the stent against and partially into the arterial wall.
APPLICATIONS OF HIGH-PRESSURE BALLOONS
Dilatation. Angioplasty is the most common application of high-pressure balloons. Percutaneous translumenal coronary angioplasty (PTCA) uses dilatation balloons to dilate and unblock arteries that feed the heart. Typical balloons for PTCA catheters range in size from 2 to 4 mm in diameter and 10 to 40 mm in length, with pressure-capability ratings of 10–20 atm. For noncoronary percutaneous translumenal angioplasty (PTA)—that is, dilatation of arteries other than the coronary arteries—balloon sizes typically range from 4 to 12 mm in diameter and 20 to 100 mm in length. Rated pressures for PTA catheters range from 8 to 20 atm.

Figure 6. Offering less precision, an elastomeric balloon (right) will often expand asymmetrically compared with a high-pressure, thin-walled balloon (left).
High-pressure balloons are also used or are being developed to dilate constrictions and blockages virtually anywhere in the body. These uses include esophageal, biliary-duct, urethral, fallopian-tube, heart-valve, tear-duct, and carpal-tunnel dilatation. Several of these procedures—like carpal-tunnel dilatation—are new and emerging (Figure 3), whereas others such as the dilatation of heart valves (valvuloplasty) have existed for many years. All of these applications benefit from high-pressure, low-compliance, low-profile balloons.
High-pressure balloons are commonly used to deploy and postdilate stents to reduce the rate of arterial restenosis or acute reclosure following angioplasty. Coronary stents—generally, machined tubes or wire mesh—are crimped over a balloon and inserted into the area of a blockage after angioplasty (Figure 4). Inflating the balloon opens the stent (Figure 5), which remains expanded to keep the vessel open after the balloon is deflated and removed from the body. The characteristics of high-pressure balloons enable the physician to fully expand a stent until it is in full contact with the arterial wall. The use of a low-compliance balloon imparts added confidence that the stent and the artery will not be overexpanded and that the balloon will not dog-bone and overexpand the artery on either end of the stent. Stents are being used with increasing frequency in association with angioplasty procedures, and currently represent the second-largest market for high-pressure balloons.

Figure 7. A directional coronary arthrectomy catheter is shown with the balloon inflated, which pushes a cutter against arterial plaque.
Positioning. A new market for high-pressure balloons is their use to precisely position devices other than stents in a vessel or body cavity. Elastomeric balloons are often used for positioning; however, high-pressure balloons are preferred when a precise balloon shape or catheter position is required. An elastomeric balloon can stretch and roll, shifting back and forth, which is unacceptable in critical positioning applications. In addition, elastomeric balloons often inflate nonconcentrically and unpredictably, which precludes their use in applications demanding extreme accuracy (Figure 6).

A variety of complex balloon shapes can be fabricated from PET to completely fill various body cavities.
A balloon can be used to center a device in a vessel, such as a radioactive seed, to deliver radiation intended to prevent restenosis. Centering the device ensures symmetrical dosage around the vessel wall. Some procedures concentrate on only one side of a vessel or cavity, such as directional arthrectomy, which cuts away plaque from the wall of a vessel using a cutter that spins at high speed inside a housing. A balloon is mounted to the back of the housing and inflated, pushing the cutter against the vessel wall (Figure 7).
Another example is the treatment of benign prostate hyperplasia (BPH), an enlargement of the prostate gland. In this application, an offset balloon can be used to position a device off to the side, directly against a lobe of the gland, to deliver microwave or laser energy only where it is needed (Figure 8). Conversely, a standard balloon can be used to ensure that the device remains centered.
High-pressure balloons are also used to position diagnostic devices inside vessels or body cavities for ultrasound imaging and other techniques. Rather than having a complicated steering or positioning mechanism on the end of a catheter, a high-pressure balloon can be used to either center or offset the device, precisely positioning it as required.
Occlusion. Normally, low-pressure, elastomeric balloons are used for occlusion or sealing, but in some cases, when precise sizes or shapes are required, it is desirable to use a high-pressure balloon. High-pressure occlusion balloons can be made shorter or longer than elastomeric balloons, thus either reducing or increasing the surface area covered in the vessel or cavity. Because high-pressure balloons can be precisely shaped, particularly in the transition area, they offer advantages over elastomeric balloons, whose ends are always spherically shaped. Conical, square, or spherical high-pressure balloons are those typically used for various occlusion applications.
KEY DEFINITIONS Balloon Diameter: Nominal inflated balloon diameter measured at a specified pressure. Balloon Length: Typically refers to the working length or the length of the straight body section. Burst Pressure: Average pressure required to rupture a balloon; usually measured at body temperature. Rated Burst Pressure: Maximum statistically guaranteed pressure to which a balloon can be inflated without failing. For PTCA and PTA catheters, this is normally at a 95% confidence/99.9% guaranteed level. Balloon Profile: Maximum diameter of the balloon when mounted on a catheter in its deflated and wrapped condition, or the smallest hole through which the deflated wrapped balloon catheter can pass. Balloon Compliance: Change in balloon diameter as a function of inflation pressure. |
Endovascular Graft Delivery. A new market for high-pressure balloons is being used in a procedure to repair aneurysms without open surgery. A balloon-mounted, woven artificial graft with a stentlike structure built in on each end or over the entire length is wrapped tightly onto the balloon to minimize its profile. The graft, which is longer than the aneurysm, is deployed and attached to the artery wall by inflating the balloon within the artery. The graft bypasses the weakened area of the artery and remains in place permanently anchored to the vessel wall, restoring normal circulatory flow after the balloon is deflated and removed.2 A wide variety of balloon diameters and lengths are required in this procedure, with tapered and otherwise custom-shaped balloons sometimes specified as well.

Figure 8. A cooling balloon used in the treatment of benign prostate hyperplasia. The black dot shown in the enlargement is a temperature sensor positioned by a small side lumen.
Light Therapy. PET balloons are optically clear and permit the transmission of light over a broad spectrum, making them well suited for laser balloon angioplasty and photodynamic therapy (PDT) with light-activated drugs (Figure 9). The simultaneous application of heat and pressure during laser balloon angioplasty of coronary arteries reduces arterial recoil, remodels thrombi into a nonobstructive film, eliminates vasospasm, and may seal minute dissections induced during conventional PTCA.3 Devices mounted inside the balloon can emit light through the balloon wall.
PDT is currently used in the treatment of Barrett's esophagus, a precancerous condition that is being experimentally treated by a light-activated drug. In this procedure, the patient is given an intravenous drug treatment one to two days before light therapy. A laser delivery device is mounted inside a specially designed balloon catheter and introduced into the patient's esophagus (Figure 10). When the balloon is inflated in the treatment area and the laser turned on, the laser light emitted through the clear "window" portion of the balloon activates the drug designed to destroy the precancerous cells. The inflated PDT balloon opens the esophagus, which is normally collapsed, and centers the laser delivery device. An opaque coating on the ends of the balloon prevents the light from treating other healthy areas of the organ, so that only the cells exposed to the light are destroyed.

Figure 9. A laser balloon angioplasty device used in coronary angioplasty. The laser is mounted inside the balloon and transmits light through the balloon walls.
Drug Delivery. Another prominent application area for high-pressure balloons is drug delivery. Use of the balloons enables physicians to localize the medication and avoid systemic intravenous administration. One method that can be used to deliver a toxic drug to a blockage or lesion is to use two discrete balloons mounted on a catheter shaft to seal off the afflicted area, while the medication is infused through a port in the catheter between the two balloons. Once the treatment is complete, the fluid is drained, the area flushed, and the balloons deflated and retracted.
A dog bone–shaped balloon can also be used to deliver drugs in a similar manner. The ends of the balloon can be of equal or different sizes, depending on the shape of the cavity or vessel. When inflated, the ends seal off the area to be treated, and the medication is infused through a hole or series of holes in the narrower center section of the balloon. The holes can be made in the surface of the balloon with a laser, hot wire, or drilling device, creating a sort of sponge. Such processing can be accomplished with virtually any balloon.
Alternatively, an ultrathin-walled PET balloon can be converted to a microporous membrane, with hole sizes ranging from less than 1 mm to several microns in diameter. Hundreds of thousands or even millions of holes of this size can be placed in a single balloon. Such a design permits pore size to be precisely controlled, enabling very small amounts of a drug to be infused over an accurately defined area—a critical advantage with drugs that are both expensive and toxic (Figures 11 and 12).

Figure 10. Balloon catheters with different-sized, optically clear "windows" used to deliver laser light energy that activates a drug for the treatment of Barrett's esophagus. The balloon ends have an opaque coating to protect adjacent tissue.
Although such balloons contain millions of micropores they are, surprisingly, very strong due to the material's unique structure. In fact, they can still be used for angioplasty: while the inflated balloon dilates the afflicted area, it can also infuse medication, perhaps delivering an anticoagulant onto the wall of the vessel. Drug absorption and penetration into the vessel wall can be controlled by the rate of fluid flow across the membrane and by the pressure at which the fluid is delivered. Through control of hole size and pattern, fluid flow can be governed and directed.
Drugs can also be coated onto the surface of a balloon for delivery to a specific site in the body. Transfer of the drug from a balloon's surface to the cavity wall can be accomplished with pressure, heat, or laser light. For example, laser and thermal energy have been used experimentally to enhance the binding of heparin to an injured arterial wall. In the experiment, lesions were treated immediately after PTCA with a laser balloon that had been coated with heparin. The results suggest that heparin therapy is a safe treatment that yields favorable acute angiographic results.3
Heat Transfer. High-pressure balloons can be used to transfer heat or cold, either into or out of a vessel or body cavity. Balloons serve as a very good medium because their ultrathin walls provide a relatively high rate of heat transfer. They also provide intimate contact with the area being treated, conforming to curves and irregularities in the surface of a vessel.
For example, in cryosurgery of the prostate, a specially designed fluid-circulating high-pressure balloon catheter is inserted in the urethra.4 The long, thin-walled balloon covers the length of the urethra up into the bladder to protect the urethra and urethral sphincter muscles from being damaged by the extreme cold produced by cryoprobes inserted in to the prostate gland. Flexibility, conformability, and high heat-transfer rates are critical to protect tissue and muscles in the application.
MULTIFUNCTIONAL BALLOONS
High-pressure balloons can be designed to perform several tasks at once—for instance, occlusion in conjunction with device positioning. An example would be a treatment for BPH that involves the application of thermal energy to the prostate with a microwave antenna inside a balloon (Figure 8). Microwave energy is emitted through the walls of the balloon, heating the prostate from the inside out as the microwaves penetrate the tissue. The antenna must be cooled during the procedure to keep it from overheating, which is achieved through administration of a cooling fluid that also cools the lining of the urethra to protect it from thermal damage. As an added function, a small side lumen is added to the cooling balloon that precisely positions a thermal sensor relative to the curve of the catheter and holds it against the tissue being treated. The sensor can be used to control the energy level of the microwave antenna and cut off power if the temperature gets too high.

Figure 11. A balloon fabricated as a microporous membrane can be designed to "weep" medication, which spreads in a thin film between the balloon and surrounding tissue.
MULTILUMEN BALLOONS
Balloons can be created with several lumens or channels so as to allow them to perform multiple functions in both the inflated and deflated state.5 For example, a balloon can be fabricated in such a way as to enable blood to flow through one or multiple lumens while the other lumens inflate to perform angioplasty. In another design, one or more of the lumens could be used to contain a diagnostic or therapeutic device (or multiple devices) for precise positioning.
CONCLUSION
High-pressure balloons, traditionally used only in angioplasty, are now being employed in a wide range of diagnostic and therapeutic devices due to improvements in materials, balloon design, and fabrication technology. These improvements include increased diameters, additional lengths, ultrathin walls (for minimal invasiveness and a smaller profile), varying diameters throughout the balloon, custom shapes, tapered ends and angles, and specialty coatings, among others. The developments in high-pressure balloon technology have resulted in multifunctional balloons that provide endless product design possibilities for the medical device design engineer. A single balloon or device can now have many functions. All of these enhancements are enabling designers to develop new and improved medical devices.
ACKNOWLEDGMENTS
The author would like to thank Michael Barbere and Ilidia Porto, both of Advanced Polymers Inc., and Victor Porto of Porto Computer Solutions for their contributions to this article. Appreciation is also extended to the companies that provided products or photographs.
REFERENCES
1. Beer and Johnston, eds., Mechanics of Materials (New York: McGraw-Hill, 1981), 325–327.
2. Baxter Healthcare, PR Newswire, August 11, 1999.
3. James J Glazier et al., "Laser Balloon Angioplasty Combined with Local Intracoronary Heparin Therapy: Immediate and Short-term Follow-up Results," American Heart Journal 134, no. 2 (1997): 266–273.
4. Mark Saab, Heat-transfer catheters and methods of making and using same, U.S. Pat. 5,624,392, April 29, 1997.
5. Mark Saab, Multilumen balloons and catheters made therewith, U.S. Pat. 5,342,301, August 30, 1994.
Mark A. Saab is president of Advanced Polymers Inc. (Salem, NH). The company manufactures ultrathin-walled heat-shrink tubing and high-pressure balloons, specializing in the design, development, and fabrication of PET angioplasty balloons and custom balloon catheters.
Back to the MDDI September table of contents | Back to the MDDI home page
Copyright ©2000 Medical Device & Diagnostic Industry
About the Author(s)
You May Also Like


