Promising in vitro diagnostic technologies could change the way one of the world's deadliest diseases is diagnosed.
March 24, 2014

It should not be surprising that the most strenuous efforts in medical science are aimed at the disease that is the No. 2 killer in the world. Cancer killed more than 7 million people worldwide in 2010, according to a report from the American Cancer Society; that’s more than AIDS, malaria, and tuberculosis combined. It is second only to heart disease as the leading cause of death across the globe. Absent a change, the number of annual cancer deaths could reach 13.2 million by 2030.
Science and medicine are turning to novel approaches in an attempt to make sure those grim projections don’t come true. Stronger cancer treatments are certainly part of development goals, but a premium is also being put on early detection to make those treatments more effective. Kalorama estimates that this focus has led to a $5.2 billion market for commercialized products to test for cancer. As one of the fastest-growing areas of in vitro diagnostics, cancer testing will grow to become an $8 billion market in 2018, Kalorama expects. Moreover, this lucrative, expansive market still has plenty of room for new entrants and better technologies.
|
Life Technologies's QuantStudio 3-D digital PCR system is currently for research only, though an FDA-cleared version can be used with Quidel flu assays. |
As important as early detection of cancer is, knowing the precise nature of what has been detected is even more essential. Continued research has shown that differing levels of gene and protein expression have a distinct link to tumor aggressiveness and therapy sensitivity. Precision medicine—quantitation, multiplexing, and highly precise identification of markers—is now the goal of cancer testing. Precise tools once thought only to be useful in a research setting are now being adopted in clinical practice.
An important first step in cancer testing was digital imaging that eliminated human discretion in reading stained-tissue slides. Digital histopathology provided an objective measure of large-scale DNA abnormalities that can indicate precancerous or cancerous changes and quantify protein expression. But as important as this development was, it did not offer enough precision. Digital histology provides a measure of quantitation, but it cannot provide quantitation down to the cellular level.
All of these techniques would be for naught if there were no way to handle the data. The arrival of high-powered bioinformatics has been essential to turning the reams of data produced by these quantitative techniques into actionable clinical information.Today, technologies in disparate fields are being used in conjunction to improve cancer testing. Refinement of laser-capture microdissection allows individual tumor cells to be picked from even the smallest tissue samples. Nanoflow techniques can separate targeted cells from the population of cells under investigation. Then, these selected cells can be further tested using sophisticated techniques including digital polymerase chain reaction (PCR), next-generation sequencing, mass spectrometry, pyrosequencing, methylation status techniques, and microarrays. These quantitative approaches are crucial to the development of truly personalized tumor analysis that more precisely reflects what is actually happening in vivo.
But even with new information technology equipment, precision medicine has not yet reached its full potential. Still, the ability to use a combination of likely technologies aided by bioinformatics to detect cancer represents an important leap forward. Among the most promising platforms are digital PCR, mass spectrometry, chromosome analysis, tissue microassays, next-generation sequencing, and cell signaling pathway testing.
Digital PCR
|
The RainDrop Digital PCR System incorporates RainStorm technology to perform biological analysis of diseases including cancer. |
Digital PCR transforms exponential and analog polychromase chain reactions into a linear, digital signal. The technology has been shown to be better than other methods at detecting subtle differences between samples with similar genomic structures. This is especially important in determining drug targets for pharmacodiagnostic testing and stratifying disease.
At this time, no digital PCR systems have been cleared for clinical diagnostics, but they are used in cancer research. Billerica, MA-based RainDance Technologies’s microdroplet-based RainStorm technology enables researchers to perform fully automated biological analysis in disease areas including cancer, infectious disease, immunology, and genetic screening. In 2012, Carlsbad, CA-based Life Technologies (acquired by Thermo Fisher Scientific early this year) introduced its QuantStudio 3-D digital PCR system, a scalable, chip-based instrument that the company says is offered at a benchtop price, potentially democratizing this technology for the rapidly growing market. The QuantStudio is used for cancer research only, though an FDA-cleared version can be used with Quidel flu assays.
Mass Spectrometry
Mass spectrometry is a separation analytical technique that identifies the chemical composition of a sample based on the mass-to-charge ratio of charged particles. Until recently, mass spectrometry was a complicated technology available exclusively to highly trained experts. The development of this technology into an accessible platform has been pioneered by companies including Bruker Biosciences, Applied Biosystems/ABX Sciex/MDS Analytical Technologies, and Sequenom.
|
Sequenom's MassARRAY uses mass spectrometry. |
Mass spectrometry analysis of proteins related to specific disease conditions in formalin-fixed, paraffin-embedded tissue and blood is opening huge opportunities in cancer diagnostics. Circulating proteins and nucleic acids present viable candidates for the characterization of the phenotypical state of an organism. Thus, mass spectrometry may assist in the detection, monitoring, and treatment of cancer. While none of the tests using mass spectrometry are used for routine patient work-up yet, some are used in research, and others aid pharmaceutical companies in drug development.
Chromosome Analysis
Abnormal chromosome content, also known as aneuploidy, has been shown to be a common characteristic of tumors and may contribute to tumor development by influencing chromosomal imbalance during cell replication. Chromosome analysis performed using fluorescence in situ hybridization (FISH) may be effective because it offers direct visual detection of abnormalities and the quantification of cells with fluorescent probes. This technique is in the early stage of development, but recent interest in this technology by Illumina, Agilent, and PerkinElmer demonstrates its potential. Still, a number of technological hurdles must be resolved. Many of the tissues and fluids from cancer patients do not provide an adequate number of cells for analysis, so using current histological techniques may result in false-negative test results.
Tissue Microarrays
The MammaPrint test measures the expression of 70 genes through microarray technology to determine how aggressive a breast cancer tumor is and gauge the patient's risk for recurrence. |
Tissue microarrays (TMAs) are used to analyze DNA, mRNA, and protein expression patterns in situ in a wide range of tissue types all on one slide. TMA sections can also be analyzed using standard pathology methods such as hematoxylin/eosin staining, immunohistochemistry, or in situ hybridization. The market for TMAs has stalled somewhat since the technology’s first big breakthroughs in the mid-2000s, but they have received more attention recently because there are a few successful commercialized tests.
Amsterdam-based Agendia’s MammaPrint test for breast cancer recurrence was the first TMA to be granted FDA clearance, which it obtained in February 2007. Offered as a test service, MammaPrint is a DNA microarray-based in vitro diagnostic laboratory service that measures the activity of 70 genes, providing information about the likelihood of tumor recurrence.
Redwood City, CA-based Genomic Health’s OncoType test for breast cancer—by far the most influential microarray-based test on the market—is also offered as a test service, as are almost all tissue arrays, with the exception of Marseille, France-based Ipsogen’s CE-Marked products.
?Next-Generation Sequencing
DNA sequencing, developed in the late 1970s, was once thought to be too cumbersome, labor-intensive, and expensive for clinical use. But next-generation sequencing with smaller, faster, and cheaper instruments and technologies that aim to put sequencing into the hands of routine labs has changed that perception. Tracking genetic differences that distinguish tumors from other tissues can help drive treatment strategies and monitor their effectiveness. Several sequencing-based diagnostic tests and test services have recently launched, including Althea Diagnostics’s BRAF mutations test, Sequenta’s LymphoSIGHT, and Enzo’s MultiGEN multiplex DNA sequencing. Pharmaceutical companies are also entering the sequencing field, and there are reports of sequencing already being used to make patient treatment decisions at large medical centers.
Cell Signaling Pathway Testing
|
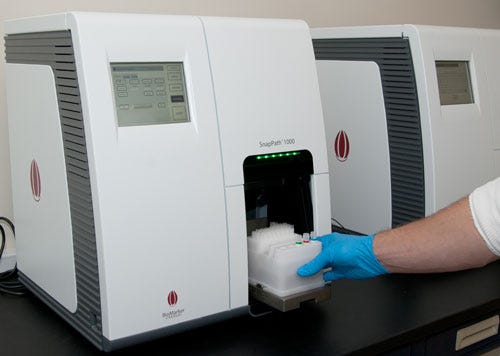
BioMarker Strategies's SnapPath system uses live tumor cells to create a functional signaling profile and is used to inform drug treatment. |
Many efforts in precision medicine have focused on the gene, and with good reason: Genes direct the production of proteins. But it is these proteins that create biological processes within a cell. Proteins also control biological communications between cells generally known as cell signaling pathways. When these pathways act abnormally, cancer can result, and drugs are being developed to block these pathways.
Researchers have begun to understand that living cells are needed to fully investigate the pathway events that lead to specific tumors. Mass spectrometry, sequencing and array technology, and sophisticated bioinformatic analysis of fixed tissues may be used to study protein function, but only functional assays on living tumor cells reveal the synthesis of this variation without the need to identify and understand every molecular variant within the network.
To this end, several research tools have been developed and are being used in test services. Baltimore-based BioMarker Strategies is developing the SnapPath system, which uses live tumor cells to create a functional signaling profile, to inform drug treatment selection for cancer patients with breast, colon, lung, pancreatic, and other solid tumors. Though cell signaling pathway testing is still in the research stage, products using this technology could represent the future of precision medicine.
The Future
Not all of the testing methods mentioned here will succeed, but it is likely that several will. There is no silver bullet test for cancer; oncologists will continue to rely on a combination of different genetic and protein biomarkers and tests to fulfill their diagnostic needs. Tissue-based testing is still the gold standard for cancer diagnosis, and biopsies will likely remain the foundation of cancer diagnosis for some time. As yet no other method currently available reveals the biological story of a patient’s cancer and all the important signs of patient outcomes.
But oncologists will also begin to correlate information from immunoassays, hematology, molecular assays, flow cytometry, and histology in their treatment plans to enhance what will surely be a primary tissue-based test. Expect to see an increasing crossfertilization of tests and technologies such as tissue-based tests with sequencing, digital PCR, and mass spectrometry. Companies are already crosslicensing technologies and collaborating on the development of more precise cancer tests.
Unless trends improve, most of the future growth for cancer diagnostics will continue to be in Western nations that have the resources for testing and treatment. The considerable investment required for this technology is not yet possible for many patients in developing healthcare systems, including the fast-growing economies of Brazil, Russia, India, and China, outside of elite-level healthcare service and medical tourism settings. Kalorama estimates that 83% of the revenue earned by testing companies will come from developed areas such as the United States, Europe, and Japan.
For the IVD industry, successful commercialization depends largely on the value proposition—especially when the cost of some molecular tests is around $600 for simple one-target tests and as high as $5000 for test panels. To bring new products to market in the current healthcare economy IVD companies will have to use the most advanced marketing techniques and demonstrate credible value for their products. A major key to success will be managing the value perception of a product in relation to the competition and the status quo in test procedures. Market value perception and competition can make or break the reimbursement proposition.
Precision tests and emerging pharmacodiagnostics are ideally suited to help physicians choose appropriate patient-specific therapies and monitor their effects. To be successful, IVD companies must demonstrate the impact their tests will have on physicians' decisions, and in doing so, they may be able to demand premium pricing for their products.
Bruce Carlson is the publisher of Kalorama Information, a provider of market research for medical markets.
You May Also Like