Neurological
Swoop portable magnetic resonance brain imaging system 
Neurological
Hyperfine Enrolls First Patients in Swoop CARE PMR StudyHyperfine Enrolls First Patients in Swoop CARE PMR Study
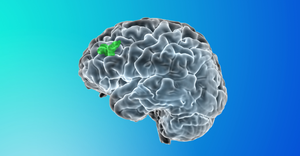
The study will evaluate whether portable MR brain imaging can reliably identify brain swelling and bleeding associated with Alzheimer’s amyloid-targeting therapy at the same time as infusions to lessen inconvenience for patients.
Sign up for the QMED & MD+DI Daily newsletter.


.png?width=700&auto=webp&quality=80&disable=upscale)
.png?width=700&auto=webp&quality=80&disable=upscale)
.png?width=700&auto=webp&quality=80&disable=upscale)
.png?width=300&auto=webp&quality=80&disable=upscale)