From microtexturing to plasma processing and electropolishing, implant surface treatment can reduce friction, remove imperfections, and improve wettability
December 7, 2011
After a medical implant or implant component has been molded, extruded, or machined, it must still undergo surface treatments to prepare it for use in the body. Surface-treatment processes can be performed for a variety of reasons, including reducing friction to decrease surface tack, removing material imperfections caused during the micromachining process, enhancing a device's corrosion resistance or biocompatibility, and improving surface wettability prior to the application of an antimicrobial coating.
To achieve these ends, surface-treatment specialists have perfected a variety of process technologies, including microtexturing to create finely roughened surfaces, plasma treatments to promote the adhesion of dissimilar materials, and electropolishing to both polish and passivate metal surfaces. In all cases, manufacturers' choice of surface-preparation methods depends on the material in question, the product design, and the device's intended end-use application.
Microstructuring Tubing Surfaces
|
|
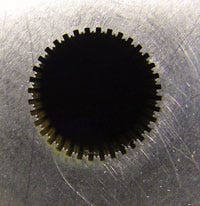
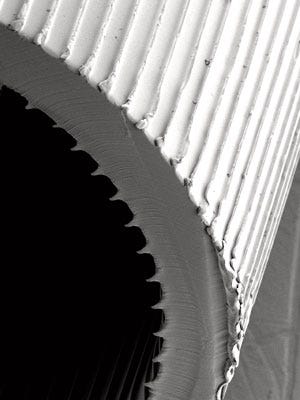
Hoowaki's microstructuring process transfers patterns from dies (top) to medical tubing (bottom). |
In many implantable medical device applications, the physician's ability to insert and remove the device easily without friction is essential. To accomplish this goal, Hoowaki LLC (Pendleton, SC) specializes in the engineering of low-friction surfaces on extrusion dies, which are used to create microstructures on the outer surfaces of medical tubing. "We modify the surfaces of industrial tooling used to extrude medical tubing featuring microstructures," remarks Sarah Hulseman, Hoowaki's product development engineer. "These features transfer from the tooling to the product during standard manufacturing processes." The company's microstructured surfaces are not coatings, Hulseman adds. Rather, they are tiny features that are directly formed into the material of the product.
Hoowaki's microstructured surfaces serve to reduce friction on the surface of medical tubing partially by reducing the tubing's area that contacts the body or other outer surfaces and partially by changing the geometry of the surface at the interface. By lowering surface friction, the technology reduces tack, making it easier for doctors to insert the tubing and reducing the potential for tissue damage.
Based on the work of William King, a professor in the nanoengineering laboratory at the University of Illinois at Urbana-Champaign, Hoowaki's microstructuring technology combines microfabrication capabilities and industrial manufacturing. Like most microstructuring technologies, the company's methods start with silicon, Hulseman explains. But then, depending on the desired feature size, the company employs several different proprietary methods for creating the microstructured surfaces.
"First, we work with our customers to understand their application and to identify the types of improvements they require on their product," Hulseman says. "We then design and engineer the appropriate surface to achieve those attributes." This process includes determining the appropriate die material and how the manufacturing process will affect the geometry of the final product. It also requires that the die undergo adjustments to achieve the correct specifications for the end product. "Generally, we are able to amend the customer's extrusion dies to achieve the desired results," Hulseman says. "We often provide engineering assistance during the initial trials, since the new tooling may require new maintenance procedures."
The company's surface-modification processes allow medical implant makers to use their preferred materials almost independently of their surface function, Hulseman comments. Based on the specific material and application, these techniques are used to custom design features, taking into account material shrinkage, drawdown, and the device's end-use application. Demonstrating up to a 15% reduction in dry sliding conditions and up to an 80% reduction in lubricated sliding conditions, Hoowaki's technique boosts the surface capabilities of standard polymers, according to Hulseman. In addition, its process can engineer the internal surfaces of tubing to improve flow or to reduce drag.
Engineered with features ranging in size from 0.8 to 400 µm, depending on the needs of the application, the company's linear or 3-D microstructured surfaces can accommodate a variety of tubing materials, including silicones, rubber, polypropylene, polyethylene, fluoropolymers, and nylon. Typical extruded tubing or device dimensions range from 0.5 to 50 mm in diameter or width.
The technology promotes process improvements as well. For example, using Hoowaki's technology, catheter manufacturers can fabricate smaller-diameter products that exhibit increased flow rates. "Our technology enables medical device and component manufacturers to enjoy performance improvements without changing their manufacturing methods," Hulseman notes.
Plasma Promotes Adhesion
In many medical implant applications, dissimilar materials must be bonded to each other. For example, coatings must adhere to device substrates, and components made from different thermoplastic polymers must be combined to form the finished device. To adhere such dissimilar materials, plasma processes are often employed to prepare material surfaces for subsequent bonding steps.
|
Plasma Etch's PE-100 system produces hydrophilic surfaces to facilitate bonding of dissimilar materials. |
But dissimilar materials often cannot be bonded easily, remarks Tom Chill, marketing manager systems engineer at Plasma Etch (Carson City, NV). To bond disparate materials, it is first necessary to create wettable surfaces, a processing step that is accomplished using plasma technology. "Our surface treatment enables significantly improved wettability prior to applying coatings or bonding materials. This capability ensures that the coating will not delaminate and prevents the parts from separating." The typical process gases used in the company's plasma processes--argon and oxygen--ensure hydrophilicity, Chill adds. "Argon mechanically removes organic contaminants from all medical devices materials, while oxygen is used to chemically react with plastic surfaces, making them very hydrophilic."
Incorporating both a plasma etching mode that can perform reactive ion etch (RIE) anisotropic-type etching and a cleaning/etching mode that can perform isotropic-type cleaning, Plasma Etch's convertible PE-100 system is used to produce hydrophilic surfaces required for adhering dissimilar materials. "Hydrophobic surfaces cause adhesives to bead off," Chill says. "Hydrophilicity does exactly the opposite. By treating plastic surfaces with oxygen, a chemical reaction takes place whereby hydroxyl sites are formed. This promotes adhesion."
The PE-100's RIE mode produces a directional plasma stream, Chill notes. This function produces high etch rates and etching patterns that allow the system to eliminate difficult-to-remove organic materials. "While RIE is primarily associated with semiconductor fabrication processing for etching patterns in integrated circuits, it can also be used to remove thick polymers and heavy organic contamination from the oils that are used in some medical device fabrication operations," Chill says. "The system's isotropic conversion electrode kit, on the other hand, enables large quantities of parts to be surface-treated in a batch process in which the plasma affects the parts from all directions."
Capable of removing organic contaminants from metals or plastics and suitable for preparing the surfaces of catheters, pacemakers, and other medical implants, Plasma Etch's surface-treatment processes are employed in a variety of prebonding applications. For example, by plasma treating a customer's polyethylene-based catheter and a polyethylene terephthalate balloon, the company was able to increase the completed device's bond strength by more than 50%, according to Chill.
Electropolishing Imperfections
The micromachining processes used to fabricate medical implantable devices such as nitinol stents often result in surface imperfections that can affect device performance in the operating room. To remove such imperfections, Pulse Systems (Concord, CA) offers electropolishing services that enhance the smoothness, corrosion resistance, and biocompatibility of implantable devices.
"The main reasons for electropolishing medical devices is to round their edges, smooth their surfaces, and improve their fatigue performance and corrosion resistance," explains Brock Groth, electropolishing manager at Pulse Systems. "Whereas electroplating adds a layer of metal to an existing part, electropolishing removes material from its surface." Electropolishing, Groth adds, removes material preferentially. "In general, more material is removed from high points than from low points, translating into edge rounding, surface smoothing, an overall reduction in the size of such features as strut widths, and an increase in the size of such features as holes."
Nitinol, according to Groth, is always covered with an oxide layer, but not all oxide layers are equal. Depending on its thickness, this layer can be amber, blue, or even dark gray. Poorly structured, such thick oxide layers are susceptible to cracking. In contrast, the oxide layer created during the electropolishing process is basically transparent, allowing the nitinol's silver color to show through. While it is thin, this well-structured layer is also durable, enabling it to bond well to the bulk material and offering a shield against corrosion. "Thin and adherent--that's the catchphrase for electropolished nitinol oxide," Groth comments.
In addition to ensuring corrosion resistance and enhancing fatigue performance, electropolishing promotes medical device biocompatibility. "When a stent is implanted in the body, blood rushes past it," Groth comments. "Anything you can do to inhibit the platelet cascade--the process that starts the formation of a blood clot--is a step you want to take. That's one example in which removing material from the surface of a component or device can pay dividends in terms of biocompatibility." Furthermore, because electropolishing passivates device surfaces, it causes devices to become more neutral toward the body, Groth adds. Because of the passivation factor, electropolishing impedes cell growth and other biological phenomena on the implant surface.
But electropolishing has yet another purpose, according to Groth: aesthetics. Surgeons associate shiny, silver objects with cleanliness, sterility, and high performance. Although a nitinol part with a blue or amber oxide surface may perform perfectly well in certain applications, those who have to handle such devices may not respond positively to them. "Looks sometimes matter," Groth adds.
To electropolish a nitinol stent, the component is first fixtured to a conductive material and then immersed in a bath containing the appropriate electrolyte and electrodes. In the bath, the part and its fixturing act as the positive side of the electrical circuit, while the electrodes are attached to a power supply with negative leads. When power is applied to the circuit, the current flows through the electrolyte via the ions that shed off the component. This process results in material removal.
Like medical devices themselves, electropolishing is specific to the application, according to Groth. For electropolishing nitinol, Pulse Systems offers four basic setups involving four different chemistries, temperatures, and power settings. Custom electropolishing options are also available. While some setups are better for removing more material, others are more suitable for removing less. While some perform well at rounding corners, others are better at maintaining dimensional ratios during electropolishing. And while some setups are used to polish inside small gaps, others are preferable for polishing component inner diameters.
"It's hard to say why one component may need lower material-removal amounts than another without knowing the function or design of the component in question," Groth remarks. "But in general terms, permanently implanted devices will likely require more material removal than devices that remain in the body for a few hours during surgery." Permanently implanted devices, Groth adds, simply have a higher bar to clear when it comes to corrosion and fatigue performance.
About the Author(s)
You May Also Like