Originally Published MDDI July 2001R&D DIGEST
July 1, 2001
Originally Published MDDI July 2001
R&D DIGEST
|
The color gradient in projected plastic samples reveals internal residual stress. |
The increasingly competitive nature of manufacturing is driving the search for technologies that offer OEMs advanced capabilities. The goal is to find ways to create products that are stronger, lighter, more cost-efficient, or less harmful to the environment. Often the key element is to explore new materials or processes. At times, however, researchers examine potential improvements in existing technologies. Work being conducted at Lehigh University (Bethlehem, PA), for example, could lead to development of injection molding processes capable of producing stronger plastic products that are also environmentally beneficial.
According to John Coulter, PhD, associate professor of mechanical engineering and mechanics at Lehigh, only a small amount of recycled plastic is used in traditional injection molding processes. This is because recycled plastic is poor in quality and would reduce the product's strength. The process uses a vibration-assisted injection molding technique to enable manufacturers to recycle previously unusable plastic but still generate products that are stronger than those manufactured with conventional means.
Other researchers have tried to vibrate heated plastic, but doing so requires costly machine or mold changes. Coulter has found that vibrating the feed screw can achieve similar results without the need to vibrate the mold. Simple changes were made to the screw's hydraulic system, and software was designed to direct the device to vibrate at low frequencies after plastic is fed into the mold.
The researcher suggests that plastics are strengthened through vibration because the motion changes their molecular orientation or alignment. Molecules in nonvibrated plastics may stick to the wall of the mold or become folded over. He speculates that vibration of the molecules mixes them more uniformly and allows them to stretch out to their entire length.
Coulter says, "If this process takes off, any company involved in injection molding could duplicate what we are doing inexpensively and probably do it better."
"Viral Angels" Treat Tumors The concept of gene therapy has received substantial attention by the mainstream media in recent years. The idea of using tiny biological agents to deliver therapeutic substances directly to disease sites has tantalized researchers and the public alike. In June, the University of Arizona College of Medicine (Tucson) was selected as the first U.S. site for a study to investigate the use of viral gene delivery to treat tumors in certain patients. The research, which will begin in January 2002, will entail use of the therapy to treat patients diagnosed with difficult-to-treat glioblastoma multiform brain tumors. Patients with such tumors must now undergo such treatments as surgery, radiation, and chemotherapy. According to Allan J. Hamilton, MD, FACS, head of the department of surgery, "One of the biggest roadblocks with current treatments is reaching and killing every last cancer cell." In the study, trillions of nonreplicating virus cells containing the beta interferon gene will be injected directly into each tumor site. The gene then causes the tumor cells to produce beta interferons, which have been shown to act as anticancer agents because of their ability to stimulate the immune system. Hamilton notes that the amount of virus injected will be smaller than a teardrop. "You know the phrase, 'How many angels can fit on the head of a pin?' Well, in this case, it's about three trillion," he says. The gene will cause the tumor cells to produce beta interferons, which act as anticancer agents. Beta interferons act as "antiangiogenic" agents, interfering with the tumor's ability to recruit blood vessels, says Hamilton. |
|
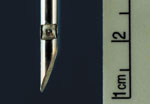
The tiny probe functions similarly to conventional transducers. |
Ultrasonic Probe Rapidly Detects Solid Tumors
A miniature probe that incorporates an ultrasonic sensor could reduce the need for surgical biopsies, which can be uncomfortable if not painful for patients. The technology, which is being developed at the University of Illinois (Champaign, IL), could also eliminate delays and stress while patients wait for lab results. "Our system could facilitate the early diagnosis of cancer," says William O'Brien Jr., professor of electrical and computer engineering and the director of the Bioacoustics Research Laboratory at the university's Beckman Institute for Advanced Science and Technology.
"When evaluating a potentially cancerous tumor, a pathologist will look for certain features in cell structure and growth pattern," said James F. Zachary, interim department head of veterinary pathobiology and collaborator on the project. "By examining the size and shape of the cells, and how they interact with surrounding tissue, a determination can be made whether the tumor is malignant or benign."
According to the researchers, the probe functions similarly to conventional transducers used in diagnostic ultrasound imaging. The tiny ultrasound transducer can be fabricated on a needle and operated in vivo at high frequencies. The researchers believe that the device will eventually be capable of resolving individual cells, including those of a solid tumor.
Operating at a frequency of 300 MHz, they say, the probe would have an image resolution comparable to what a pathologist sees when examining tissue under a microscope. The pathologist could thus use the minimally invasive procedure to achieve the same goal as a surgical biopsy. Says Zachary, "By inserting the probe into a tumor and displaying the image on a monitor, we could identify and classify the tumor in real time. We could also send the image over the Internet to specific specialists for help in identification."
To achieve the target frequency of 300 MHz, transducers are being fabricated from a new type of high-strain piezoelectric material that can provide sufficient electromechanical efficiency for the ultrasonic microprobe. The piezocrystals were grown using a modified flux growth method. "This material has the potential for being extremely efficient, but it's also very fragile," O'Brien says. "The thinner the crystal, the higher the frequency response—and that has presented certain mechanical difficulties." A fabrication process has also been developed for the proposed ultrasonic probe.
|
Ultrasonic transducers can be fabricated on needles for in vivo applications. |
The researchers state that progress is being made on three major parts of the project. Miniature probes that work at up to 70 MHz have been created, functional image-formation techniques have been devised, and a database of ultrasound images of both tumors and healthy tissue has been developed. "We still need to push the transducer frequency response up to 300 MHz, and we need to make the probes much smaller," O'Brien explains. "Ultimately, we want to mount the transducer on the end of an acupuncture needle. That way, when the probe is inserted, the patient will feel no pain."
According to Mark A. Haun, who is assisting on the project, "A variety of synthetic-aperture and tomographic imaging techniques are being explored to reconstruct the three-dimensional tissue volume surrounding such a probe." He adds that methods will also be explored to compensate for phase errors caused by tissue inhomogeneities, as required for coherent imaging. Other challenges caused by the nonlinear propagation of sound may also need to be addressed. Haun says, "One imaging concept uses a single focused transducer on the surface of a needle and builds on earlier work with synthetic-aperture image formation with virtual sources."
|
Research led by Mitrani is focused on creating "microlivers" to function as temporary organ replacements. |
Micro-Organs Used for Artificial Livers
Attempts to create a system capable of temporarily replacing essential liver function have centered around using cells harvested from pigs. The porcine liver cells are suspended in a matrix within a container to filter and detoxify a patient's blood. Now, researchers led by Eduardo Mitrani, PhD, of the Alexander Silberman Institute of Life Sciences at the Hebrew University of Jerusalem, are exploring the application of micro-organ technology in developing a bioartificial liver.
The technique enables the researchers to cultivate micro-organs ex vivo, using animal or human cells, to form an array of "micro-livers" that can function as a temporary normal liver. Mitrani recently received the university's Kaye Prize for his achievements. According to the researchers, micro-organ technology allows virtually any type of normal cell to be grown in the laboratory under conditions similar to those existing within the body.
Ordinarily, cells grown in laboratory dishes, isolated from their normal environment, lose some of their specialized functions. Studies of cells taken from various organs using the new technology, however, have shown that the cells continue to function ex vivo and can express tissue-specific genes for long periods.
One practical application of micro-organ technology is the development of the extracorporeal liver device, which will serve as a bridge to transplant or to restore function until the patient's liver regenerates. The liver device, called aLIVE, has been tested successfully on animals and human studies are now planned.
Other applications of the micro-organ technology are being explored as well. Among these are a bioartificial kidney; a genetically engineered biopump that would be worn under the skin and would supply any recombinant protein, such as growth hormone, to a patient who lacks it; and an implanted, cell-based angiopump that would promote formation of new blood vessels from the patient's own tissues.
MRI Technique Relies on Noble Gases to Detect Lung Disease
Research being conducted at the University of Virginia Health System (Charlottesville, VA) could yield an improved imaging technique for detecting such lung diseases as asthma, emphysema, and cystic fibrosis. By detecting such conditions at an earlier stage, when treatment is more likely to be effective, the technology could help hold down healthcare costs and prevent many of the more than 350,000 lung-related deaths in the United States each year.
The new technique, which entails in vivo magnetic resonance imaging (MRI) using new imaging agents called hyperpolarized noble gases, is being developed by James R. Brookeman, professor of radiology and biomedical engineering, and John P. Mugler III, associate professor of radiology and biomedical engineering. According to Brookeman, the procedure can detect subtle ventilation defects in the lung that are not visible with any other medical imaging procedure. Image acquisition requires only a short breath-holding procedure that uses about a liter of a specially prepared gas such as helium or xenon.
Says Brookeman, "The key difference between helium 3 and xenon 129 is that helium is virtually insoluble in any human tissue or fluid and so does not accumulate and is easily exhaled, whereas xenon is fairly soluble, particularly in blood and lipid tissues; it is easily carried from the lungs to the brain; and at lung concentrations above 30%, is an anesthetic." He explains that the properties displayed by xenon may provide specific diagnostic advantages. "This solubility holds out the possibility of hyperpolarized xenon being used to study brain perfusion," he adds.
More than 200 human lung studies have been completed, says Brookeman. "The current results for asthma are very promising, and could point the way to develop and refine new asthma therapies, particularly for children." He believes that such results with the noble-gas method "will undoubtedly stimulate numerous applications in the medical field and beyond."
Brookeman also predicts that future studies could involve conventional proton MRI with T1-weighted, T2-weighted, and diffusion-weighted images. "We anticipate that hyperpolarized noble-gas MRI will have a series of image types such as a ventilation image, where the gas goes at equilibrium; an apparent diffusion coefficient image, which provides information on the lung microstructure; and a dynamic image, in which an image is acquired every 10 milliseconds, to show how the gas sequentially distributes in the lung."
The potential benefits of the technique are speculative but promising, according to Brookeman. "At the moment there is greater diagnostic accuracy, but at greater cost," he explains. "However, the technology is new and on a steep learning curve," he adds.
Says Brookman, "It could be that cheaper, special low-field MR imagers could be developed that would permit patients to stand up, like in a chest x-ray, and hold their breath for 10 seconds after inhaling the polarized gas, and this would provide a complete functional lung study."
Copyright ©2001 Medical Device & Diagnostic Industry
You May Also Like