Healthcare is revving up for remote patient monitoring. But can the current infrastructure support it?
May 9, 2022

Although remote patient monitoring (RPM) in the healthcare setting is seeing exciting growth, some practitioners and patients are not realizing the true potential for achieving worldwide wellness. According to an April 2022 Arizton Advisory and Intelligence report, the global RPM market will reach $62 billion by 2027, from $30.5 billion in 2021. So, while the worldwide CAGR is a healthy 12.5%, it could be better. RPM device manufacturers, healthcare providers, and their patients, and the technology that binds them can create an environment where the future of RPM, jumpstarted by COVID-19, will continue to grow and thrive.
Pros and cons of RPM
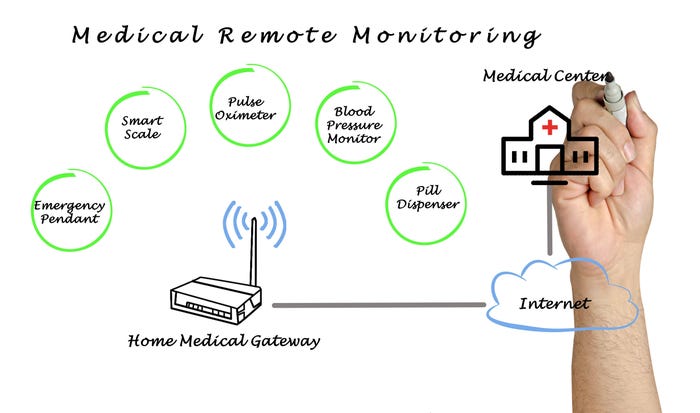
On the plus side, RPM devices offer lower healthcare delivery costs, expanded access to medical advances, and innovative ways of addressing the aging population with stay-at-home information transfer. The recent COVID-19 pandemic opened acceptance of these technologies to new populations, which could lead to an overall boost in world health.
Under the minus column, some patients are simply unaware of the existence of RPM and therefore don’t have access to the knowledge they need. Also, in some cases, RPM increases the possibility of fraudulent charges by healthcare providers and exposes patients to improper data handling, including data security and privacy. For these reasons, it’s no surprise that patients are hesitant to adopt “new” technology when they don’t see the benefits outweighing the risks.
Reaching industry growth estimates depends on a trusting partnership between device manufacturers and health care providers (HCPs) and their patients. However, the invisible—but perhaps most important—partner is the connecting tissue of the cloud surrounding the interactions. How can the RPM partnership of manufacturers + HCPs + patients + technology create trust here? Is engaging newer players—startup manufacturers or younger HCPs and patients—the answer? Not necessarily. Nor are they the short-term target markets for the change. Today’s aging and inaccessible populations need the benefits offered by RPM devices sooner rather than later. The solution will be to assess the technology appropriately and safely pair it with healthcare processes in a value chain that connects everyone concerned.
How RPMs change the healthcare delivery dynamic
Professionals who develop, design, and manufacture medical products that comply with complex and demanding regulations and market requirements work tirelessly to improve outcomes. “Improving outcomes” can range from better capturing of the data moving between the HCP and their patients to enhancing the interface for the technologically challenged, either from the user’s age or from their previous experience with devices of any kind. “Remote” can mean patients don’t have to drive their cars to the provider’s location, or it can mean a patient is in a remote place, for example, across the world. The delivery dynamic often means the patient takes responsibility for monitoring their device and taking medications as prescribed so that the HCP can see it’s been done. Another delivery dynamic occurs when the patient takes their heart monitor or sleep recording device back to the doctor’s office or drops it in the mail in a pre-addressed, postage-paid envelope. The variations on the theme are endless, yet the industry could be doing more sooner. Both legacy and new players will approach RPM solutions differently.
Market overview: companies and devices
The industry’s legacy players enjoy the lion’s share of the market. Yet newer, scrappier startups are making inroads in the marketplace. Legacy companies include Baxter (founded in 1931), Dexcom (1999), Honeywell (1906), Medtronic (1949), Philips Healthcare (1891), as well as American Telecare; Roche; Bosch; Biotronik; Intel; Welch Allyn; Health Anywhere Inc.; Johnson & Johnson; and Covidien. Some newer companies include Gyant, ChroniSense Medical, Ejenta, Cardiomo Inc., 100Plus, Vitls, Neteera, Cu-Bix, iHealth, and Health Recovery Solutions (see below).
RPM is used in a number of market segments to manage chronic disease, blood pressure, brain monitoring, breath rate, glucose levels, hematology, heart rate, vital signs, and specialty monitors for fetal heart rate, prothrombin, multi-parameter, and more. In addition to utilization by HCPs and their patients, RPM can be used in home care settings, clinics, long-term care centers, and hospitals.
The RPM industry mimics others in that the big guys and little guys co-exist and compete for market share. It is hoped that this David and Goliath contest results in a greater good from the synergy of everyone’s desire to help improve patient outcomes. Each player, large and small, has its strong and weak points. Are the Goliaths too slow or too blind to react, as Malcolm Gladwell would have you believe in his book David and Goliath? Are the “David” startups loose cannons?
Legacy RPMs
Legacy RPM device manufacturers bring deep pockets for R&D. They convey experience and leverage their permanence to attract great minds toward solving today’s healthcare challenges. Equalizing global access to healthcare is a challenge being handled by remote patient monitoring. Passing patient data electronically to and from the HCP sites (i.e., hospitals, testing and treatment sites) radicalizes the exchange. The medical device and diagnostic industry is accustomed to seeing big RPM device companies supply big hospitals, which in turn interact with big pharmaceutical firms, selling their products, devices, and solutions to each other through big supply chains. Are these big companies delivering on their promises? Is the patient still the center of their energies?
Big firms attract money, medical and scientific advances, and experience to their doors. Teaching hospitals and long-term care facilities as well as rehabilitation campuses with a history of patient care and good recovery records have all contributed to the level of healthcare enjoyed in the United States. Society needs Goliath-big legacy companies and David-small companies, too.
Startup RPMs
Startups and smaller companies help the industry thrive and grow by being nimbler, requiring fewer rules, and allowing them to pivot faster. But also, their devices and services often bind HCPs and patients in more meaningful ways. The “unicorns” bring fresh eyes to revitalize the connective tissue between providers and patients even if it’s through technology.
The startup groups in the RPM space are making inroads. Forbes Magazine published an article about Health Recovery Solutions, a new company that recorded patients’ vitals and transmitted them to clinicians via Bluetooth through instant messaging or video. The 34-year-old founder, Jarrett Barrett, began thinking about the company in 2012, but his idea finally took roots in 2020. During the worst of the COVID-19 pandemic, hundreds of patients, including his grandmother, could be cared for remotely when no hospital beds could be found. His mission is to partner "with health systems in a way that stops people from coming into hospitals.”
Health Recovery Solutions is one of many small companies altering the dynamic of healthcare by combining telehealth/telemedicine and RPM technology within a larger collection of digital health tools. Investors are flocking to their door. According to Barrett, the company’s business model works this way: “The company makes money by billing clinical institutions on subscription to integrate their solutions in treatment, coming at no additional cost to patients.”
Is big better?
According to the Peter G. Peterson Foundation, “Even before the pandemic, the United States spent a significant portion of its resources on healthcare without generating better outcomes” [emphasis added]. The foundation’s article summarizes the report from the Economic Co-operation and Development’s (OECD) 2020 Health Statistics, and includes data that compares healthcare spending in the United States to that of other countries. The report is pre-pandemic, making it a “cleaner” example of a healthcare system that isn’t working very well.
Minding the gaps
North America has the largest RPM system market share globally. According to the Peterson Foundation report, the United States spends significantly more per person on healthcare than other developed countries. Despite this, healthcare outcomes for some basic health problems are worse. Experts believe that increased use of RPM devices should address both matters: patient outcomes should improve and delivery costs should decrease—a win-win. Improved patient outcomes need to be the driving force, but how is the task going to work in the real world?
Better systems
According to the Centers for Disease Control and Prevention (CDC), chronic diseases account for 90% of total healthcare costs in the United States each year. Patients want to believe they’re at the epicenter of healthcare systems. Yet, the systems that surround U.S. healthcare make the costs higher than in other countries and they’re increasing. The Peter G. Peterson Foundation states, “in 2020, the U.S. devoted 20% of its economy to healthcare. Such a large proportion of resources dedicated to healthcare makes it increasingly difficult to invest in other sectors of our economy.” Even so, some systems are working well.
HCPs are increasingly turning to digital solutions to increase care and keep costs down. Statistista.com reports that according to a survey conducted in the United States in April 2021, 60% of physicians had recommended the use of electronic health records to their patients, while a further 57% had recommended using remote/virtual consultation with a healthcare professional.
Original equipment manufacturers (OEMs) and startups seek ways to make smarter devices and easier paths between their patients and their data, their diseases, and their treatments.
When global health is the focus, everyone wins. The pie doesn’t need to get bigger for people to feel better. The pie needs to be cut equally. The United States needs better outcomes at lower prices. The rest of the world needs our access to healthcare at prices they can afford.
Overcoming risks and optimizing usage
Remote patient monitoring can help stem the increase in healthcare costs by catching problems sooner, reducing the need for emergency care in some cases, handling chronic diseases more efficiently, and enabling feedback loops and continuous tracking between patients and providers. Higher frequency of monitoring (weekly, daily, hourly, continuous) through AI-assisted data capture, diagnosis, and treatment will yield lower delivery and administrative costs. Patients can be more compliant because they know they’re “being watched,” but also, they don’t have to guess. “Did I take my morning pills or not? Did I remember my insulin?” The monitor knows all. But perhaps too much.
In an increasingly digital world, the privacy of patient records is paramount. Every player in the RPM system, including the patient, must be honest. HCPs and the participants within the healthcare bubble must adhere to safe data handling standards from HIPAA and other regulations. For the system to work, unscrupulous billing cannot be tolerated. All the watches, bracelets, handhelds, tablet computers, mobile phones, and high-tech gadgets and gizmos are only as good as the people using them. And the patients will not use them if they do not trust the system.
Improving lives and outcomes
It’s exciting to see cardiac, neurological, respiratory, neonatal, and many more monitoring devices saving lives. The next trend in RPM technology is miniaturization, as device manufacturers make their solutions smaller and less invasive, while partnering with new players to expand their ingenuity and market share.
Still, the patient needs to be at the center of the RPM circle. The profit motive is excellent for engaging exploration, R&D, clinical trials, expansion, and experimentation as this brave new world of devices multiplies globally. Yet, the profit motive needs its own remote monitoring, and the monitoring cannot come only from outside. It’s an inside job that derives from some sense of discipline surrounding the interplay among the HCPs, RPM device manufacturers, and cloud platforms. The benefits for society are worth that effort.
RPMs shift us toward improved quality of life, driving better patient outcomes. The ultimate goal is to enhance healthcare providers’ ability to act as change agents to increase RPM usage across the patient care ecosystem. Self-monitored participants in the RPM/telehealth marketplace can make remote patient monitoring safe and healthy for everyone. Revving up for RPMs will provide better outcomes for the United States and help the health community worldwide.
About the Author:
Abhishek Sinha is a business and integration architect manager for Accenture, LLP with more than 16 years’ experience in pharmaceutical, automobile, and e-commerce digital enterprise solutions. He can be reached at [email protected] or on LinkedIn.
About the Author(s)
You May Also Like


