Identifying opportunities for device innovation to reduce and prevent hospital-acquired infections.
August 19, 2015

Identifying opportunities for device innovation to reduce and prevent healthcare-associated infections.
Sue MacInnes
Why the buzz around bugs?
There was a time when being in the hospital was considered the best place to be if you had an infection or had some type of medical complication. The best minds and science were surrounding you, so—whew—you were in a “safe” place. At that time, a certain amount of infections were just plain “unavoidable” in healthcare speak. They were a part of what happens when you are sick or are having some kind of medical procedure.
It wasn’t until the 1999 Institute of Medicine (IOM) report, “To Err Is Human,” that the public learned about the 98,000 medical errors that occur in hospitals annually and the fact that you were more likely to die from an error in a hospital than in an airline crash. Yet, there was almost no publicity about the adverse activities that happened every day in healthcare. In fact, I was recently at a conference where one of the authors of the report stated that the number was closer to 200,000 but they chose to be conservative and only included data that was reported and published.
Over fifteen years later, healthcare has changed, regulations have changed, and infections within healthcare systems are measured by the number of infections, not just the rate, because each infection is a person. That person could be you or I, a friend, or a relative . . . and that person matters. Evidence shows that healthcare-associated infections (HAIs) can be prevented and the related financial burden can be reduced by millions, perhaps billions, of dollars.
To add further incentive, the Affordable Care Act (ACA) has three different elements that can penalize hospitals by as much as 6% of their Medicare revenue. Each of the three elements, Value Based Purchasing, Readmissions, and the Hospital Acquired Conditions program were a direct result of the IOM report and the need to improve quality, cost, and the healthcare experience for the American consumer.
Innovation Fights Infection—What Are the Needs and How Do You Do It?
New devices can bring exciting innovations and changes to current protocols. However, when dealing with healthcare there are several things that are crucial to the success of any new device. Here is the short list:
1. Show evidence that your new design works.
2. Show that it supports best practice.
3. Show that it reduces costs.
4. Show that it improves outcomes.
All are possible and within reach. The word in healthcare that innovators need to be aware of is “evidence-based." Features and benefits of any new product will fall on deaf ears if you do not supply the background information proving that your product works. In this new world of healthcare not only does the product have to work but you will need to figure out how to train or educate the user.
Products are going home with patients . . . patients and family members will need to be educated in a very consumer-friendly way. Healthcare has not been geared toward consumers in the past so this is an opportunity to not only innovate but to bring the product to life by paying attention to patient/staff education on the product.
As you research the market and the needs here are a few suggestions:
1.Do your homework. Know which infections are the most prevalent and what they cost. Three out of four HAIs in the acute care setting are a result of one of these four infections:
•Catheter Associated Blood Stream Infections (CLABSI)
•Catheter Associated Urinary Tract Infections (CAUTI)
•Surgical Site Infections (SSI)
•Pneumonia
New emphasis will soon be placed on C.diff and MRSA as both conditions will be included in the financial metrics supported by the ACA. To further emphasize the importance of these infections to cost, quality, and the patient experience, the federal government has written these infections into law. In other words, hospitals across the country are being rated against each other, their infection data is transparent and available to the public, and their Medicare payments are now being dramatically influenced by where they rank. A deep surgical site infection is documented as adding $27,407 in additional costs. This infection is one of the major reasons for hospital readmissions, which are also penalized.
More than half of the nation’s academic medical centers have been fined for excessive infection and medical complications resulting in a readmission within 30 days of discharge. Another thing to note is that even if a hospital does well one year, the government continues to change the metrics every year, adding new complications and infections while at the same time hospitals struggle to maintain numbers that will keep them out of the penalty box. One CEO likens this to a game of whack-a-mole. Targets keep changing, penalties keep changing, and competing hospitals that are also striving to improve numbers create further pressure.
2.What constitutes “costs” associated with HAIs? HAIs can create excessive financial burdens. Some of the areas affected are prolonged hospital stays, log-term disabilities, increased resistance to microorganisms to antimicrobial agents, massive additional financial burden for the health system, high costs for patients and their families, and excessive deaths.
3.Where do HAIs occur? They happen at acute care hospitals, outpatient clinics, surgery centers, dialysis centers, nursing homes, and other places throughout the continuum of care. It's worth noting that some areas like dialysis and surgery centers do not have the infrastructure to have sufficient infection control practices in place.
4.What are some of the reasons for HAIs? The list can be long. To name a few:
1.The placement of medical devices such as a catheter, i.e., prolonged inappropriate use of these devices and antibiotics
2.High risk and sophisticated procedures
3. Undergoing surgery
4. A lengthy hospital stay
5. Transmissions between patients and healthcare workers (inappropriate use of standard and isolation precautions)
Even more important are human factors and variance in practice. New devices to support the reduction in infections need to consider processes, education, and training that support evidence or building products that prevent or reduce human error.
5.How can I find clues to innovation opportunities?
Do a deep dive into the subject. First, learn everything you can about a particular infection. Many infections have guidelines from the CDC or professional organizations. Know the guidelines and proper prophylaxis. The National Institutes of Health has published many “bundles” to help prevent infections. These bundles pool together evidence-based information that supports different ideal conditions. Basically, there is not one cure or preventative treatment to reduce infections; there are many contributing variables.
This is also documented well by The Joint Commission Center for Transforming Healthcare as they collaborate with large healthcare systems using lean principals to uncover the barriers and individual issues that are considered contributing factors to infections. Knowing the contributing factors gives the entrepreneur a world of inside information from which to build.
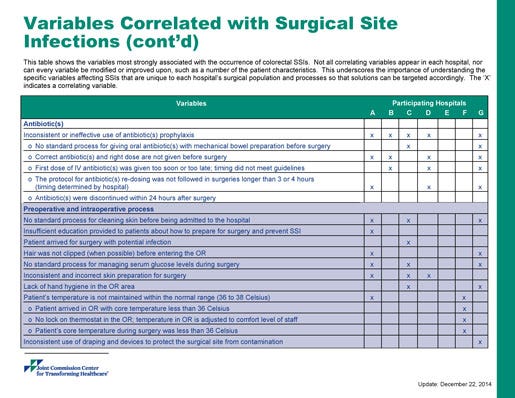
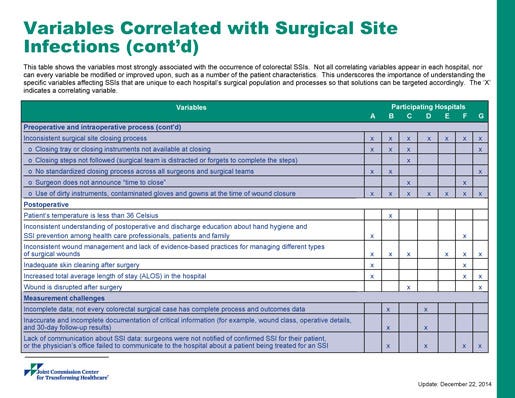
These charts detail an example of one project on colorectal surgical site infections from The Joint Commission Center for Transforming Healthcare.
Other opportunities come from the new models of healthcare like accountable care organizations (ACOs), where providers are responsible for health needs of a population of people. In this model, the focus goes beyond the acute care walls to the providers in the continuum (home health, urgent care centers, clinics, surgery centers, long-term care, etc). Keeping populations well and promoting wellness supports the health of the ACO.
Many hospitals are doing joint ventures with retail stores like Walgreens, CVS, and Walmart to provide minute clinics and convenient patient access to healthcare. Thus, consumer-oriented support can promote an entirely new opportunity being driven by large integrated delivery networks and their associated heath plans.
Health systems are narrowing their networks, looking for new innovations to promote wellness, and identifying new solutions to reduce infections and complications. Yes, there is science to be studied and learned, but equally important is understanding human behavior, observing current practices of care, and seeking out-of-the-box solutions. Healthcare is lacking innovation, the understanding of consumer behavior, and insight into the variance of current practices of healthcare workers . . . all of which provide the answers to new device design.
Sue MacInnes is chief market solutions officer at Medline Industries, Inc. Reach her at [email protected]
Learn more from MacInnes at MEDevice San Diego, September 1–2, 2015, in San Diego. She'll be giving a keynote address on "Putting Superbug Infections Under the Innovation Microscope: Identifying Hospitals' Top HAI Needs for New Device Solutions" on Sept. 2. |
[Images courtesy of IDEA GO/FREEDIGITALPHOTOS.NET and THE JOINT COMMISSION CENTER FOR TRANSFORMING HEALTHCARE]
You May Also Like


