The design and engineering story behind Molli, a wire-free localization technology for breast cancer surgery.
May 1, 2021
Editor's note: This is part one of a two-part story on Molli Surgical's recently FDA-cleared technology. Part one covers the design and engineering process, while part two focuses on the clinician and patient experience of the technology.
Ananth Ravi, PhD, was a newly-minted radiation oncology medical physicist at Sunnybrook Odette Cancer Center and clinical operations lead of brachytherapy, a hybrid of radiation oncology and surgery, when he attended a weekend barbecue that would ultimately lead to the development of a wire-free localization technology for breast cancer surgery that uses cutting-edge magnetic technology – not radioactive seeds.
“I was over at a barbecue on a weekend, believe it or not, and over a couple of hot dogs the VP of the cancer center came and tasked myself and a surgeon, [Nicole Look Hong, MD], to go out and create a better experience for patients during breast-conserving surgery," Ravi told MD+DI. "And at the time, I didn't really understand what that meant ... so he gave us a little bit of funding, and said 'go ahead and go build this.'"
The need for such a technology was really highlighted to Ravi when he later attended a patient-family advisory council meeting at which the hospital administrator is there, along with patients who shared their story and talked about their experience with breast cancer surgery. He still remembers one patient in particular who said she had arrived at the hospital first thing in the morning, and clinicians placed a wire into her breast — a common pre-surgery practice known as wire-localization, which helps the surgeon locate the tumor or lesion that needs to be removed — and the woman had been fasting for 24 hours because she was scheduled to have the surgery that day. The problem is that Sunnybrook is a very busy trauma center, so her surgery kept getting delayed.
"And she was there in pain with this wire in place, she was anxious not knowing when she was going into the OR, and her story just drove home the need," Ravi said. "I was like, ‘how is this a thing? We need to figure out something that is simple, patient-centric, and an alternative to this strategy.’”
Ravi is now a c-founder and the chief science and clinical officer at Toronto, Ontario-based Molli Surgical. In developing the Molli System, he partnered with John Dillon, who served as the research engineer on the project and is also now the co-founder and chief technology officer at the company.
What was the design and engineering process like?
Through pure Edisonian trial-and-error fashion, the team kept iterating until they found a solution to the problem, in order to improve the patient experience for breast cancer surgery. The team also drew on their experience of dealing with really complex medical technologies, and Ravi understood the importance of keeping the design of the solution as simple as possible.
"If you have too many widgets, and too many buttons, and too many complicated workflows, the likelihood of there being a mistake or something breaking when you need it to work the most is very high," Ravi said. "So that became part of our design ethos ... patient-centered care is the ultimate goal of what every practitioner wants to do — and when I was in the clinic that's what I wanted to do — but you have to balance. You have to balance cost, patient wait times, administrative overflow paperwork, and then at the end with COVID-19 there is so much burnout that's happening.
As clinicians and hospital administrators work to balance all of those things simultaneously, the focus is no longer just on the patient experience. So Ravi and his team committed early on to making sure that whatever technology they were going to implement would be simple, easy to use, and robust. That's how Molli was born.
"We went through multiple iterations, and a number of different technologies, and what we decided was that we were not going to let the technology drive the solution," Ravi said. "It has to be custom-fitted, tailored to the solution, to be the simplest way of solving the problem."
Ravi chuckled as he said the development process also involved a couple of lab fires, "thanks to John blowing up a couple of capacitators."
"One of the key challenges through these iterations was the dogged pursuit [to find] the simplest, most robust technologies out there," Ravi said.
The team started off with technologies that they soon realized would have failed after only a couple uses because they just weren't robust enough. Other technologies they tried would have created issues with interference with other surgical instruments in the operating room.
"When you think about it, you're trying to find a way to be able to detect some signal, and there's only so many different types of electromagnetic signals you can choose from, and you're always fighting with physics against things that can interfere with what's used in the OR," said Fazila Seker, PhD, president and CEO at Molli Surgical. "So when I think back to all the different designs that Ananth and John's team went through, it was really around different types of physics principles for detection, and they finally landed on what Molli is, and that is permanent magnetism."
Because of that permanent magnetism, Seker explained, the system is able to be used alongside standard metal surgical instruments because the team designed that detection system, and the algorithm that goes into it, in such a way that it eliminates that potential for interference that would have been an issue with some of the earlier iterations they experimented with.
"And when you think about it, you also have lighting in the OR, right? So certain methods suffer from interference with lighting in the OR," Seker said. "What does that translate into? That can translate into errors in the readouts, the distances, and that could translate into potential errors in the margins for the actual tumor excision."
Ravi also pointed out that the operating room is not a gentle environment, given the speed and the efficiency that is required of the operating room staff, so surgical devices and equipment used in the operating room are really put through the paces, he said. That meant his team had to build a technology that would hold up under those conditions.
"And to Fazila's point, we tested every part of the electromagnetic spectrum for a potential solution, and this one was the one that kind of resonated the most because the technology we have is also robust, and it wasn't something you had to handle with kid gloves, [or something that] if you breathed on it, it would break," he said.
So having an iterative design and engineering process was really key to the team's ultimate success.
And those many iterations and lab fires were clearly all worth it in the end, because the company now has an FDA-cleared product that checks all of the boxes Ravi mentioned in terms of being simple to implement, with a very low learning curve, while also improving the patient experience. Molli is truly a medical device that makes breast cancer surgery (and breast-conserving surgery at that) precise, and helps surgeons locate even the smallest tumors with unprecedented precision, Ravi said.
So what exactly is Molli?
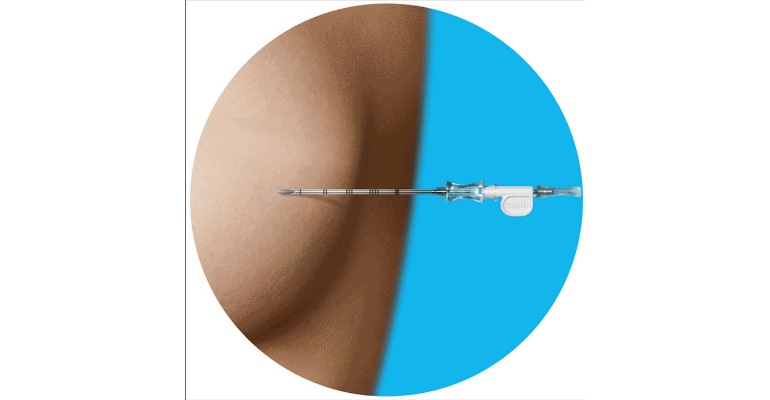
The Molli System is a wire-free localization technology for breast cancer surgery that consists of three components. The first component is an implantable magnetic marker (non-radioactive) just 3.2 millimeters in size that is designed to mark the location of the tumor. The second component of the system is a wand designed to detect that marker (and therefore the tumor). The third component is a visualization tablet that the wand connects to in order to give readout of the distance between the tip of the wand and the implanted marker. The magnetic marker can be placed into the breast, either at the time of surgery, or up to 30 days in advance.
Colloquially, Ravi said, the magic is in the detection wand because the wand is designed to provide a distance measurement with millimeter accuracy in locating the marker. He also said that, because the marker is so tiny, it allows surgeons to provide the best optimal cosmetic outcomes for the patient, as well as an effective therapeutic outcome.
Unlike radioactive seed localization methods, Ravi said Molli eliminates any anxiety patients may have related to radiation exposure. He also notes that because Molli is based on magnetism, not radiation, hospitals avoid the time-consuming, and expensive resources required to adhere to radiation safety regulations.
"With Molli, there are no complex monitoring and disposal protocols, cumbersome and expensive equipment, or lost time searching for a misplaced radioactive seed," Ravi said.
So easy a 3-year-old child can do it
"The first prototype we ever made, I said, 'We have to make it so that my 3-year-old can pick it up and use it," Ravi said. "And she totally did, she found her marker in a phantom model."
That translates into a very short learning curve for both radiologists and surgeons. Ravi told MD+DI he took a piece of chicken breast into the clinic and asked radiologists to insert the magnetic marker into the chicken breast, in order to observe their learning curve. All it took was one time for them to feel like they could use the device in a field clinical case, he said.
"We didn't reinvent the wheel. I went and spent some time observing the types of introducing devices they use clinically, and we built something that was exactly like that form factor, so it was a non-issue," he said. "From the surgical perspective, it was a similar strategy. We knew some of the tools and probes that they were using, observed them in use, and then replicated that. We had one surgeon up and running within one case, another three. It really depends on their comfort using a wire-free technology. Most say you can do it within five cases, some say a single case."
About the Author(s)
You May Also Like




