FDA gave the medtech industry draft guidance on additive manufacturing earlier this year, but how can manufacturers translate the agency's thoughts into their process validation and quality assurance practices?
September 23, 2016

FDA gave the medtech industry draft guidance on additive manufacturing earlier this year, but how can manufacturers translate the agency's thoughts into their process validation and quality assurance practices?

A few months ago, FDA issued draft guidance on additive manufacturing for medical devices. This document offered industry a better idea of the agency's thinking on the use of 3-D printing and additive manufacturing for devices, but didn't give manufacturers an exact map for navigating these relatively new waters.
As a group of legal experts wrote in MD+DI soon after the draft guidance was released:
The draft guidance includes important information about FDA's current thinking, but also stops short of clearly addressing many key questions raised by the use of AM in medical devices, such as where one draws the line between the manufacturing process and the finished regulated device, considerations for point-of-care manufacturing, or who should be considered the "manufacturer" of the finished device under different scenarios."
Still, the draft document is enough to start changing some practices for device manufacturers. Mark Cola, president and CEO of Sigma Labs, pointed out during an interview this summer that process validation is one part of the manufacturing process that is evolving. Before the guidance, a manufacturing engineer took a slow, meticulous, trial-and-error approach to process validation, he said. That approach focused on the post-process portion of the manufacturing timeline.
Learn more about "FDA Regulations Impacting Connected Health Devices and IoT" at BIOMEDevice San Jose, December 7-8. |
"[Manufacturing engineers] would have to effectively make the parts in one step and inspect them in another. They would make a bunch of parts, destroy them by evaluating their strength, toughness, and other properties, fatigue resistance, as well as measuring the microstructural attributes of the part, including the geometric properties," Cola explained.
That meant that manufacturing and inspection were separate steps, causing a time lag. FDA is aware of the inefficiency and wasted resources associated with this method, Cola said. With the draft guidance, "[FDA is] trying to couple the inspection step with the manufacturing step . . . they're trying to give comfort that the entire manufacturing process is observed and not just a snapshot in time," he explained.
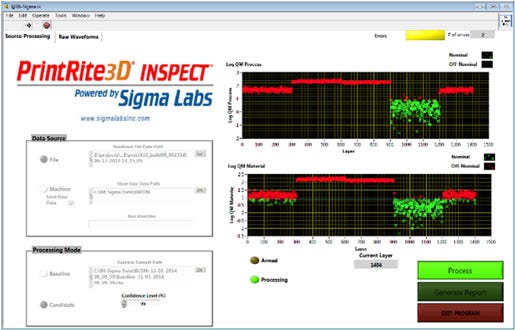
Sigma Labs' PrintRite3D system allows manufacturing engineers to perform in-process quality assurance.
Performing process validation and acceptance activities means manufacturers must show that the finished part meets design intent. There are three basic attributes--metallurgical, geometric, and mechanical properties--that need to be correct in order to show compliance with design intent.
Sigma Labs' PrintRite3D system targets the metallurgical and geometric properties, ensuring these attributes are correct in a medical device part. "Our software suite is designed to interrogate those attributes and report on every layer of every part of every build," Cola said.
|
Cola |
PrintRite3D gives manufacturing engineers near real-time information. They receive in-process quality details for each layer, giving them the opportunity to "take immediate action," Cola pointed out. After the part is finished, the engineers have an exact record of each layer of the part. "We go the extra step and we basically give the manufacturing engineer insight into the process and it repeatability, build to build and machine to machine," he said.
FDA's draft guidance recommends using test coupons, defined by the agency as "a representative test sample of the device or component," for process validation. Cola said that in that same vein, the PrintRite3D system provides "witness coupons." These "become a record of the build and provide a link back to the quality and repeatability of the process," he explained.
"Our unique selling point comes from the fact that we've gone to the trouble of taking the information we gather and [made] it actionable for the end-user, the manufacturing engineer on the floor," said Cola.
So far, feedback on the system from the medical device industry has been positive, said Ronald Fisher, vice president of business development at Sigma and head of the PrintRite3D operating division. He added that customers have mentioned that the software for monitoring geometric properties has been particularly helpful for a specific application: meeting ASTM standards for the size, shape, and depth of the pores of a surface coating. Porous, rough surface coatings are sometimes applied to implants to encourage bone growth. Some customers are "us[ing PrintRite3D] as a method of ensuring the quality of the pore structure that they're printing and producing in their final part," Fisher said.
While FDA's draft guidance addresses additive manufacturing for medical devices, Cola noted that the mass production implied by additive manufacturing is a large leap from the small volumes 3-D printing is known for. Sigma Labs' software is intended "to bridge that technology chasm and enable . . . [the] end-user to move from 3-D printing and batch production and smoothly transition over to additive manufacturing."
The agency's draft document is also helping to close that gap, Cola said. "Things like the FDA guidelines bascially pave that bridge that we've established with our software."
[Images courtesy of STUART MILES/FREEDIGITALPHOTOS.NET and SIGMA LABS]
About the Author(s)
You May Also Like



