LimFlow is touting recent results from a pilot study of its system, which is designed to switch blood flow from a blocked artery in the leg to a nearby vein to restore circulation.
August 8, 2017
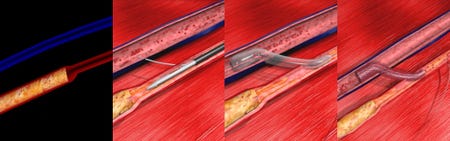
The LimFlow procedure uses two ultrasound-guided catheters, one venous and one arterial, to create an arterio-venous crossing. A stent is then used to connect the artery and the vein.
Patients at risk for lower-limb amputation from advanced peripheral arterial disease (PAD) may have another option.
Paris-based LimFlow SA has developed a minimally invasive system to switch blood flow from a blocked artery in the leg to a nearby vein to restore circulation to a blood-starved foot. The system is designed for patients who have end-stage critical limb ischemia and have exhausted all other options, including endovascular surgery.
"They have a wound on their foot that is not healing" due to lack of blood flow, explained LimFlow CEO Dan Rose. "As long as the wound is open, they're at risk of infection, sepsis, and death."
Patients with end-stage critical limb ischemia are at high risk for amputation, and many never walk again, Rose said. Most are already in some stage of sepsis when amputation is considered, and survival rates after amputation are low due to sepsis and comorbidities, he added.
LimFlow recently reported positive results from a pilot study of its system on seven elderly diabetic patients with end-stage critical limb ischemia. The company reported no deaths, above-the ankle amputations or major reinterventions at 30 days. Patients' wounds began to heal, and their at-rest pain subsided, according to the study, published in the July issue of the Journal of Endovascular Therapy.
At six months, six of seven patients had avoided major amputation, and at 12 months, five of seven had done so. Four achieved complete wound healing at six months and five did so at 12 months. The median healing time was 4.6 months. Blood circulation through tissues in the foot rose dramatically from 8 mmHG pre-procedure to 59 mmHG (p=0.080) at the time of healing.
How It Works |
An interventional cardiologist or vascular surgeon accustomed to interventional procedures inserts a catheter into the blocked artery and another into a nearby vein. Both catheters are equipped with ultrasound to communicate the site of the blockage. The physician then passes a needle from the arterial catheter to the venous one, deploys a guide wire through the needle and a covered nitinol stent to connect the artery and vein. LimFlow also developed a tiny tool to break down the valves in the vein that keep the blood flowing only in one direction so that blood can flow through the vein to the foot. |
The biggest challenge in developing the system was figuring out how to detect the best place to cross from the artery to the vein, according to Rose, a former Medtronic executive. Once both catheters are deployed, the physician rotates the arterial catheter until it produces the strongest ultrasound signal in the venous catheter.
"The whole concept is the leveraging techniques and technologies that have been used in other applications endovascularly and put it in such a way that it is adapted to the needs of our procedure," Rose said. "It's really about adapting, for the unique purpose, (percutaneous coronary intervention) technology and enabling a procedure to take place in a very reproducible, percutaneous way."
LimFlow's system received the CE Mark in October 2016. FDA granted the company an investigational device exemption in April 2017 to begin a feasibility study of 10 patients in the United States. That study began in July and should be complete in September, Rose said. The company plans to request FDA approval this fall for a pivotal trial.
Rose estimates that most of the market for this system will be elderly.
"It's a lot of 65-to-75-year-olds, people who are suffering from long time diabetic, longtime arterial disease," Rose said. "Our mission is basically to take these patients who are at the end of their therapeutic options and give them a chance to heal up and get going."
Nancy Crotti is a contributor to Qmed.
[Image credit: LimFlow SA]
About the Author(s)
You May Also Like


