If Medical Devices Could Talk to Each Other, It Would Save More Than $30 Billion A Year
Medical device interpoerability could bring us significant savings and improve patient safety, a new analysis suggests.

It's no longer an issue of something that would be nice to have.
It's actually costing us dollars and cents - and significant amounts of it.
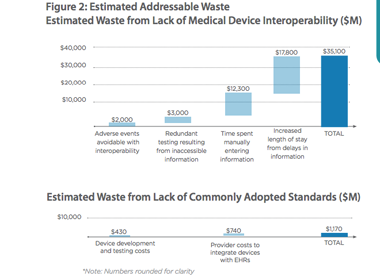
A new analysis from the nonprofit medical research group West Health Institute says that if medical devices were able to talk to one another, it would bring cost savings of more than $30 billion a year.
|
Source: The Value of Medical Device Interoperability |
Yes, medical device interoperability - something that device vendors historically have paid scant attention to - could save us roughly $36 billion annually. Not to mention help to improve patient safety.
The analysis was part of Congressional testimony that West Health Institute's Dr. Joseph Smith gave Wednesday before the House Energy and Commerce Subcommittee on Health. Smith also highlighted the regulatory and policy changes required to create the integrated, interoperable systems that would improve outcomes, lower costs while creating a higher-value health care where the patient is front and center.
"We see an enormous opportunity to use information technology and device innovation to bring about the much needed transformation in health care delivery," Smith told the subcommittee. "Today's hospitals are filled with medical devices that are unable to share critical data, creating potential dangers to patients, as well as inefficiencies that put a tremendous financial burden on our health care system," Smith said. "
Here's a portion from "The Value of Medical Device Interoperability" analysis that device firms should cringe at reading:
According to a recent report by HIMSS Analytics, while over 90 percent of the hospitals surveyed by HIMSS use six or more types of devices that could be integrated with EHRs (such as defibrillators, electrocardiographs, vital signs monitors, ventilators and infusion pumps) only a third of hospitals actually integrate medical devices with EHRs today. Additionally, those that are investing in interoperability integrate fewer than three types of devices on average, a far cry from the six to twelve devices that may be present around an intensive care unit (ICU) bed. This lack of interoperability creates significant sources of waste and risk to patient safety because of incomplete or stale information clinicians must rely on for workflow and decision making.
The problem, the report states, is that medical device firms lack the incentives and the imperatives to undertake the costly investment in medical device interoperability. As a result, the onus is on hospitals to muddle through given their own tight budgets to get these systems to talk to one another.
The analysis does not shy away from the fact that interoperability is expensive. It states that the "cost of medical device integration has been estimated at as much as $6,500 to $10,000 per bed in one-time costs, plus as much as 15 percent in annual maintenance fees."
Still the benefits should outweigh cost considerations. Here are the four areas where we would see cost savings
quality improvement through reduction of adverse events due to safety interlocks ($2 billion)
reduced cost of care secondary to avoidance of redundant testing ($3 billion)
increased clinician productivity secondary to decreased time spent manually entering information ($12 billion)
increased capacity for treatment secondary to shortening length of stay ($18 billion)
To read the full analysis, click here.
-- Arundhati Parmar, Senior Editor, MD+DI
Related Content
At HIMSS, Interoperability Calls Shotgun
$10 Device Enables Interoperability and Wireless Data Transmission
0 0 1 7 44 UBM Canon 1 1 50 14.0 Normal 0 false false false EN-US JA X-NONE
About the Author(s)
You May Also Like

.png?width=300&auto=webp&quality=80&disable=upscale)
